How your hip works
Your hip is a very stable and strong joint.
It’s known as a ball-and-socket joint. This is because the top of the thigh bone is shaped like a ball. This ‘ball’ sits inside a hollow socket in your pelvis.
Ball-and-socket joints give the most movement of all the different types of joints in the body.
The hip joint is held together by a covering of muscles which are secured to the bones by strong cords called tendons.
These muscles and tendons form a capsule around the joint and support its movements. They help move the joint, supporting your leg and upper body movement.
Inside the capsule is the synovium, which lubricates the joint with synovial fluid and keeps the cartilage healthy. The cartilage sits between the bones of your hip joint to stop them rubbing together and reduces any impact when you walk or move your hip.
With all this support, it is unusual for the hip to become dislocated, even after a high-impact injury.
When to see a doctor
Most of the time you can treat your hip pain yourself with simple self-help treatments. If your pain is extremely bad or hasn’t improved after two weeks of regularly taking painkillers, you should see your doctor.
You should see your doctor straight away if:
- you’ve had a fall or injured your hip
- the pain is getting worse
- you’re having difficulty with daily activities, for example walking, going up stairs or leaning forwards when sitting
- you feel feverish or unwell, or you’ve been losing weight.
Causes
Most of the time there is a very simple explanation for hip pain, for example if you’ve overdone it while exercising. In this case your pain is usually caused by strained or inflamed soft tissues, such as tendons, and it often clears up within a few days.
Long-term hip pain can be caused by specific conditions.
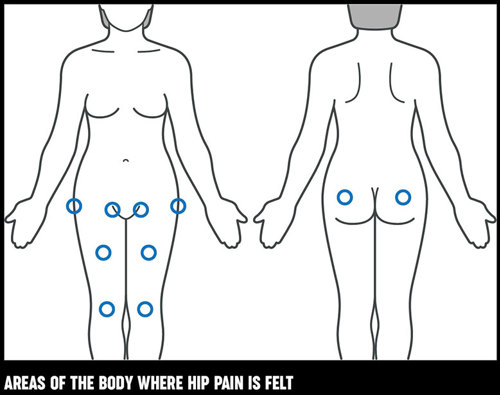
If you have a problem with your hip joint you may feel pain in the groin, down the front of the leg and in the knee. Sometimes knee pain is the only sign of a hip problem – this is called referred pain or radiated pain and is fairly common.
You may feel pain on the outside of your hip or in your buttock – though this can also be caused by problems with your lower back.
Diagnosis
If your hip pain hasn’t improved after two weeks you should see your doctor.
It’s a good idea to make some notes about your condition before you go, so you can be sure to discuss everything that’s bothering you.
Your doctor will ask about your pain and what movements make it feel worse. They’ll ask how your symptoms started, how they affect your daily activities and whether you’re in pain at night.
Pain when you bend your hip going up or down the stairs or when you put on your socks is often a sign of a hip problem.
They’ll examine your hip to find out how well it moves, and this will usually give them enough information to plan your treatment. But you may need other tests to diagnose some conditions.
What tests are there?
X-rays
X-rays are often the best way of finding out what’s wrong with your hip as they show the condition of the bones. They may also show problems in your pelvis which could explain your pain. They’re not as useful for looking at the soft tissues around the joint.
CT scans
A CT (computerised tomography) scan can often be very helpful to work out if the hip joint has an unusual shape. CT scans use x-rays to show sections or ‘slices’ of the hip, which a computer then puts together to form a 3D image of the hip.
There are conditions where the socket of the hip can be very shallow, and a CT scan can show this.
MRI scans
MRI (magnetic resonance imaging) scans use radio waves to build a picture to show what’s happening to the soft tissue, such as the muscles and tendons, inside your hip. They’re particularly helpful for diagnosing the painful condition avascular necrosis, which reduces the flow of blood to the ends of bone, causing them to collapse (See Specific hip conditions section for more information).
Blood tests
If your doctor thinks your pain is caused by an infection or rheumatoid arthritis, blood tests can often help.
Treatment
If your hip pain doesn’t improve with simple medications such as paracetamol and ibuprofen, and a mixture of rest and gentle exercises, you should see your doctor for further advice. They may recommend the following treatments:
Drugs
Non-steroidal anti-inflammatory drugs (NSAIDs)
Your doctor may prescribe stronger NSAIDs, such as diclofenac, naproxen, or a higher dose of ibuprofen, to help ease your pain.
Like all drugs, NSAIDs can sometimes have side-effects. If you’re taking prescription NSAIDs your doctor will take precautions to reduce the risk of these – for example, by prescribing the lowest effective dose for the shortest time.
Bisphosphonates
Bisphosphonates are used to treat Paget’s disease of the bone and osteoporosis. They work by slowing bone loss, which reduces the risk of hip fractures.
Physiotherapy
A physiotherapist may be able to help get your hip moving by showing you gentle range of movement exercises and activities, specific to your condition.
They are trained specialist who can show you how to help reduce your hip pain and how to improve the way your hip works in future by using a variety of strengthening and stretching exercise, massage and other therapeutic techniques.
They’ll work with you to help get your hip moving properly again. Their approach will depend on whether your problem is short-term or a long-standing condition. Almost everyone will benefit from physiotherapy, and they can recommend things such as:
- exercises to strengthen weakened muscles, change co-ordination and improve function
- advice on improving your posture
- exercises to ease or prevent stiffness
- exercises to increase the range of joint movement
- putting adhesive tape on the skin to reduce the strain on the tissues, and to help increase your awareness of the position of your hips and back
- manual treatments to the soft tissues and joints – such as massage and manipulation
- how to walk when your hip hurts
- how to use a walking stick or crutch.
It can take a while to get your referral to an NHS physiotherapist. You could see one quicker if you go privately but you’ll have to pay for this. You can find more information about private physiotherapists in your area on the Chartered Society of Physiotherapy website.
Occupational therapy
If you think your work or certain activities might be the main cause of your pain, it’s worth discussing this with an occupational therapist.
An occupational therapist is a specialist trained to help you regain your independence by showing you how to change the way you do things. They can also advise you on how equipment or adaptations could reduce the strain on your hip at home, work, or while you’re driving.
They’ll be able to give you advice on how to change your movements to help prevent pain continuing or returning. If your place of work has an occupational health department, they may also be able to help.
You can also see an occupational therapist privately. You’ll be able to get an appointment quicker, but it will cost you money. The Royal College of Occupational Therapists website can help you find a private occupational therapist in your area.
Your GP or hospital consultant can refer you for physiotherapy and occupational therapy, or you may be able to refer yourself.
Steroid injections
If your pain has been caused by bursitis or inflammation in or around your hip, steroid injections can help.
A They’re often given with a local anaesthetic which numbs the area to reduce the pain of the injection. They are usually very helpful in treating conditions affecting the trochanteric area on the outside of the hip.
Sometimes they’re also effective for treating iliopsoas tendonitis – though the injection will need to be given by a radiologist using ultrasound, because the iliopsoas tendon is so deep.
A radiologist is a doctor who specialises in imaging techniques – like x-rays, MRI and ultrasound imaging – and forms a diagnosis from the results. They can use ultrasound to pinpoint the place that a steroid injection would be most effective.
A snapping iliopsoas tendon can also be treated with steroid injections with the guidance of a type of x-ray, called video fluoroscopy, to make sure it’s given in the right place. Ultrasound-guided injections are also becoming more popular.
Surgery
Not everybody with hip pain will need surgery. Hip fractures however, almost always need surgery to stabilise the bone and hold it in place. Replacement of the ball of the hip may also be necessary.
It’s common for older people to experience hip fractures, which can take a long time to fully recover from. People can often be in hospital for a couple of weeks or more to get over the fall and subsequent operation, and many often need extra help at home after discharge.
Hip replacement surgery
If your hip pain is caused by arthritis and other treatments haven’t helped, your doctor may talk to you about hip replacement surgery. The modern techniques used in a hip replacement make the surgery very safe and people usually have extremely good outcomes after it.
- More than 90% of people who have a hip replacement find their pain is greatly reduced.
- A modern artificial hip should last at least 15 years.
Usually, you’ll only need to stay in hospital for a few days after surgery. Physiotherapists will help get your hip moving again by showing you simple exercises and ways to do daily activities.
If you’re being considered for hip replacement surgery, it’s important you’re in good health and try to keep your weight down.
Your general health will probably be assessed during a hospital appointment before, and your surgeon will also talk to you about the operation. You may also meet the physiotherapists and occupational therapists who’ll be involved in your treatment after surgery.
Revision surgery
If your hip replacement becomes loose, infected or otherwise fails, it can be corrected with further surgery. Modern revision surgery techniques are developing quickly, and most failed hip replacements can be dealt with.
You’ll be in hospital longer than your first hip replacement, and it might take longer to recover.
Acetabular labrum surgery
Surgery to reshape the hip can improve your ability to move the joint and reduce your pain and stiffness. In some cases, this procedure is performed using keyhole surgery as a hospital day case or you may stay a night in hospital.
You’ll need between one and two months off work. We don’t currently know whether this operation can stop arthritis developing in your hip.
Managing symptoms
There are several ways you can help your hip pain such as using painkillers, exercising and reducing the strain on your hip.
Painkillers
Simple painkillers or non-steroidal anti-inflammatory drugs (NSAIDs) such as paracetamol or ibuprofen tablets or gels – from a chemist or supermarket can help. A pharmacist should be able to give you good advice on what could work best for your condition. But don’t use them for more than two weeks without speaking to your GP.
You can try rubbing anti-inflammatory creams or gels onto affected areas, but some hip problems are so deep within the joint that this may not help. A pharmacist can advise you on what’s best for your condition.
Exercise
Your hip pain may improve with a few days’ rest, but as soon as the pain begins to ease, start some gentle exercise to keep your muscles working and stop your hip getting stiff.
If you don’t start moving your hip, it could start to get weaker and less flexible, which will reduce your ability to get out and about and lead a full life.
Simple exercises can also help keep the muscles strong, which will provide support to your hip and improve your symptoms. There are examples of exercises you can try on our exercises for the hips page.
Before you begin, it’s a good idea to get advice from a doctor, physiotherapist or personal trainer in a gym about specific exercises. Start by exercising very gently and build up gradually.
As with any physical activity, it’s normal to feel some discomfort or aching in your muscles after exercising. But you should stop if you get any joint pain that doesn’t go away quickly.
As well as doing specific exercises to help your hip, it’s a good idea to try to improve your general fitness. Things like going on a daily walk or going swimming will help to improve your general health and take the strain off your hip, by strengthening other muscles in the body.
Sometimes people stop exercising once their pain clears up, but when they do it’s common for them to start having problems again quite quickly. Even if you’re feeling better, it’s important you keep exercising regularly to stop the pain coming back.
Reducing the strain
It’s generally best to carry on doing your normal activities – but try not to overdo things. You might need to pace yourself and do a little more each day. There are ways you can do some daily activities slightly differently, so you don’t hurt your hip.
- Avoid sitting in low chairs as this bends the hip more and might increase your pain.
- Don’t carry heavy weights. When you’re shopping try using a trolley if it’s uncomfortable to carry a basket.
- Lessen the strain on your hip at work by finding a comfortable sitting position. Your workplace might be able to provide a footrest, back support or other equipment to help you. You could ask for a workstation assessment and talk about your condition.
- Talk to your line manager or HR department about any parts of your job you’re struggling with.
- Ask an occupational therapist or your GP whether using a walking stick could make it easier to get about. They can advise you on the correct length and the best way to use the stick.
- Lose weight if you’re overweight – your hip carries a lot of weight, so taking steps to reduce this will help.
- Avoid standing on one leg – for example, when you get into a car, sit on the side of the seat and swing both legs in rather than stepping in one leg at a time.
Complementary therapies
There are several complementary treatments that some people find relieve their hip pain. Some are available on the NHS, such as acupuncture. But there isn’t a lot of evidence, so they’re not always available on the NHS.
Complementary treatments are usually relatively safe. But, you should always talk to your doctor before you start using them in case they interfere with specific treatments.
Before starting any therapy or treatment, it’s important to make sure the therapist or supplier has a set ethical code, is legally registered and fully insured.
We have more information about the organisations that oversee complimentary treatment practitioners and what you should expect from complementary and alternative therapists.
Because you will, more than likely, be paying for any complementary treatments, you should consider whether or not they’re helping your condition before deciding if you’re going to keep using them.
We have information on complementary treatments, including acupuncture, aromatherapy, manipulative therapies – such as chiropractic or osteopathy treatments, supplements, and much more.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.
Specific hip conditions
Some of the specific conditions that affect the hip are:
Osteoarthritis
Osteoarthritis is one of the most common causes of hip pain in adults. It mainly affects the joints in the fingers, knees and hips.
Your hip joint can become painful, swollen and stiff because OA thins the cartilage that stops your bones rubbing together and causes bony lumps known as osteophytes to form on the bones of the joint.
You can feel a great deal of pain from osteoarthritis of the hip which can restrict your movement and sometimes makes you limp.
Osteoarthritis of the hip can cause a great deal of pain, restricted movement and a limp. In extreme situations, the leg can become shorter and the hip can become fixed in a bent position, making movement difficult.
For more information, see our section on osteoarthritis.
Paget’s disease of bone
Paget’s disease affects the way bone develops and renews itself, causing it to become weaker. It usually affects the pelvis, causing it to grow out of shape. This can often lead to hip pain, but it is treatable with a group of drugs called bisphosphonates.
Bisphosphonates are drugs used to prevent the loss of bone mass and treat bone disorders such as osteoporosis and Paget’s disease.
For more information see our sections on Paget’s disease and bisphosphonates.
Other types of arthritis
Inflammatory conditions, such as rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis can all cause hip pain. This can be managed with specific medications for each condition.
For more information see our sections on rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis.
Hip fractures
If you’ve fallen and hurt your hip you should see your doctor urgently, as fractures around the hip are very common, particularly in elderly people with osteoporosis.
Osteoporosis makes bones less dense and fragile, so they break or fracture more easily. You may need surgery to fix the damage.
For more information see our section on osteoporosis.
Avascular necrosis (osteonecrosis)
Avascular necrosis is a rare and painful condition that can affect any joint in the body in young-to-middle-aged adults. It occurs in the hip when the blood supply to the ball at the end of the thigh bone is lost. This causes the bone to die and the ball to collapse, which results in arthritis.
This could be a permanent or temporary loss of blood flow. Sometimes steroid treatment, for illnesses like cancer or asthma, can cause avascular necrosis as a side-effect. Alternatively, you could have a really bad fracture that affects the flow of blood to the end of the bone.
This loss of blood flow causes the bone and the tissue around it to gradually die – changing the shape of the ball at the end of the bone and making your hip painful and stiff. It can cause the ball in the joint to collapse, which results in arthritis.
It’s often referred to as idiopathic, which means that it doesn’t have any clear cause. However, it’s linked with the following:
- Drinking too much alcohol.
- Long-term use of high doses corticosteroids, such as prednisone.
- Sickle cell disease (an inherited condition that stops red blood cells from carrying oxygen through the body properly).
- Radiotherapy.
If your doctor thinks you have avascular necrosis, it’s important they refer you for an urgent MRI scan to confirm the diagnosis. As soon as you have a diagnosis, you can start treatment, which may stop the condition causing any more damage and stop you developing arthritis.
Femoroacetabular impingement (FAI)
Femoroacetabular impingement (FAI), is a condition where the ball and socket don’t move freely through their normal range of movement. This may be because the top of the ball isn’t completely round or because the socket is too deep.
It’s not fully understood why this happens, and in most circumstances no specific treatment is needed.
In some cases, surgery can improve the range of movement in the hip, but it’s not clear whether this helps prevent arthritis developing in the long-term.
If x-rays and scans of the hip joint are normal, then the symptoms may be caused by referred pain from the back. Pain caused by a problem with the lower back may only be felt in the buttocks, down the back of the legs, over the outer side of the hip joint and occasionally in the front of the hip.
Soft tissue conditions
Lateral hip pain
There are a number of conditions that can affect the outside of your hip joint. Your diagnosis will depend on how wide the affected area is.
Trochanteric bursitis
Bursae are small fluid-filled pouches, which act like cushions to reduce friction where parts of the body move over one another, for example where tendons or ligaments pass over bones.
If you have tenderness over the bony part of your hip joint, you may have trochanteric bursitis. This is caused by inflammation of the bursa at the top of the thighbone. Inflammation is a normal reaction to infection or injury and causes the bursa to become swollen, hot and painful.
It’s a very common condition, but there’s usually no obvious cause. You may just feel pain over this bony point, but it can spread down the leg or it may seem to be coming from the hip joint itself.
Trochanteric bursitis often happens in both hips. It usually improves with rest, painkillers and physiotherapy.
Very occasionally the condition can last for longer than expected, and it’s sometimes linked to problems with the area of the lower back known as the lumbar spine. Paying attention to your posture can make a big difference. The condition is common and often chronic and in many cases it’s an over-looked diagnosis.
It’s now known to affect your muscles and tendons around the trochanteric area as well, not just the bursa. This can mean you may be referred to a specialist in sports medicine, orthopaedics, rheumatology or spinal medicine.
There are also now a number of names given to this condition, depending on what type of doctor diagnoses it and how wide the area affected is. You may be told you have greater trochanter pain syndrome, trochanteric tendinobursitis or gluteal tendinopathy.
Iliopsoas tendonitis
Iliopsoas tendonitis is inflammation of the iliopsoas tendon that runs over the edge of the pelvis and helps you bend your leg up. This usually gets better on its own.
Snapping iliopsoas tendon
A snapping iliopsoas tendon doesn’t usually cause hip pain. ‘Snapping’ refers to a clicking noise you may be aware of as the tendon flicks over the edge of your pelvis when you move, it doesn’t mean the tendon breaks.
Some people say the sensation feels like their hip is popping out of place. If your doctor thinks you have this condition they’ll usually recommend you rest and use painkillers until it settles. Tests and surgery are rarely needed.
Torn acetabular labrum
The acetabular labrum is a thick ring of cartilage around the hip socket. It can be torn if the ball or socket of the hip are misshapen. This can be the result of hip problems in childhood or changes to the shape of the hip as it develops, but in most cases the cause is unknown.
If the ball of the hip joint is affected, it’s called a cam lesion. When the socket is affected, it’s known as a pincer lesion. We don’t yet know whether treating these problems with surgery prevents you from getting osteoarthritis in later life.
If your doctor thinks you have a torn acetabular labrum, they may recommend you have an arthrogram investigation. This is where a small amount of dye is injected into the hip joint before an MRI or CT scan. This gives a clear image of the surface of the bones, soft tissues and cartilage in the joint.
Other causes of groin pain
Groin pain is very commonly caused by problems with the hip. However, it can also be a symptom of other conditions, such as:
- a hernia – a painful lump, often in the groin, which may need surgery
- lymph nodes in the groin – these usually occur if there’s infection in the lower leg
- gynaecological problems, which can occasionally be felt as hip pain.
Surgery
Not everybody with hip pain will need surgery, but hip fractures almost always need fixation, which stabilises the bone and helps it to heal, or replacement of the ball of the hip. Hip fractures often occur in elderly people, and they can take a long time to fully recover from. People can often be in hospital for a couple of weeks or more to get over the fall and the operation, and many often need extra help at home after discharge.
Hip replacement surgery
If your hip pain is caused by arthritis and it’s getting worse, your doctor may talk to you about hip replacement.
Hip replacement is an extremely good treatment for arthritis-related hip pain, and modern techniques make the operation very safe with good outcomes.
Nowadays, many people only need to stay in hospital for a few days after their hip replacement, but it may be helpful if somebody is available to stay with you for a couple of weeks as your mobility and confidence improves. Physiotherapists will help you become mobile when you’re in hospital, and they’ll help you practise getting in and out of bed, out of chairs and up and down stairs safely.
If you’re being considered for hip replacement, it’s important that you’re in good health before the operation.
You’ll probably be referred to the hospital for an assessment before the operation and they’ll check your general health.
Your surgeon will talk to you about the operation itself, and you’ll meet the physiotherapists and occupational therapists who’ll be involved in your treatment after surgery.
The outcomes of hip replacements are extremely good – 90% or more of people who have had a hip replacement find their pain is greatly reduced. Modern hip replacements should last many years – around 80% of cemented hips should last for 20 years.
Revision surgery
If your hip replacement becomes loose, infected or otherwise fails, it’s possible to have surgical treatment. Modern revision surgery techniques are developing quickly and most failed hip replacements can be dealt with, which can restore function and activity.
Revision surgery is carried out by specialists in the field. You’ll be in hospital longer than for your first hip replacement, and it might take longer to recover. You’ll need physiotherapy after revision surgery to help you gain confidence in your new joint, and you’ll need someone to help you out for a couple of weeks or more when you go home.
Acetabular labrum surgery
A torn acetabular labrum can be repaired by surgical reshaping of the hip. In some cases this procedure can be performed through just a small incision (arthroscopically), so your joint doesn’t have to be opened up. This is also known as keyhole surgery, and it can be done as a day case or one-night stay in hospital.
You’ll need between one and two months off work.
We don’t yet know what the long-term effects of acetabular labrum surgery are, but you may get better hip movement as a result of it.
Research and new developments
Our research has shown that certain occupations, such as farming, can put you at greater risk of developing hip osteoarthritis.
Because of this hip osteoarthritis in farmers and other high-risk jobs is now recognised as an occupational injury, which entitles these people to claim Industrial Injuries Disablement Benefit.
We're currently funding research into developing new techniques to measure hip shape and abnormalities in babies and children.
Children with hip problems are more likely to develop osteoarthritis and to need hip replacement surgeries as young adults. This study will develop a tool to identify children who would most benefit from treatment as early as possible, reducing long-term pain and disability.
Researchers at our Centre for Sport, Exercise and Osteoarthritis are also studying the reasons why hip pain is commonly seen in young footballers.
We're also funding research looking into whether it is possible to predict the success of joint replacement surgery by looking at genetic risk factors.
This study will help doctors understand which patients are most likely to have good outcomes from joint replacement. It aims to improve patients’ experiences of surgery and make their new joints last longer.
Our researchers are also developing a tool to help patients make informed decisions about their treatment according to their lifestyle and needs.