What is osteoarthritis of the foot and ankle?
Osteoarthritis (os-tee-o-arth-ri-tis) is the most common type of arthritis. It mostly affects the hands, knees, hips and spine, but it can happen in any joint in the body, including the feet and ankles.
A joint is a part of the body where two or more bones meet. Your ankle joint is where the tibia and fibula bones in your leg join up with your foot. There are 33 joints in the foot, but the big toe is the one that is most commonly affected by osteoarthritis.
The joints in your body go through a normal cycle of damage and repair during your lifetime. But sometimes the process your body goes through to repair joints can change their shape or structure. When these changes happen in one or more of your joints, it’s called osteoarthritis.
The ends of our bones are covered in a tough but slippery surface, known as cartilage. This allows the bones to move against each other. The bones are held in place by ligaments. Tendons attached to our muscles and bones help us to move around.
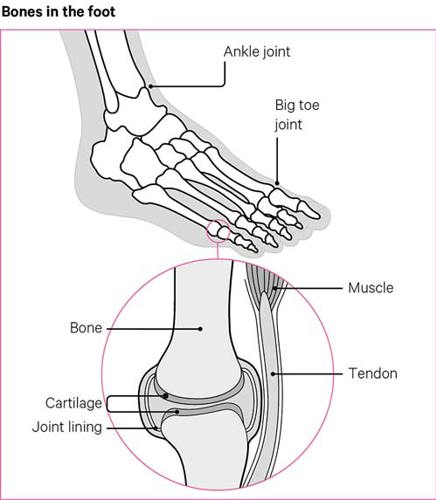
Osteoarthritis causes damage to the cartilage, which results in pain and swelling, and can sometimes mean the bones rub against each other as we move. Osteoarthritis doesn’t just affect the cartilage, but can also cause damage to the bones, ligaments, tendons and lining of affected joints.
Osteoarthritis can affect anyone at any age, but it’s most common in people over 45. It affects more women than men. The risk of developing osteoarthritis is commonly linked to:
- being overweight or obese
- your genetics, or if you have a family member with osteoarthritis
- having a condition that affects the joints, such as rheumatoid arthritis or gout.
Joint injuries can also make you more likely to get osteoarthritis, and this is particularly the case with ankle injuries.
How will it affect me?
Osteoarthritis can affect people in different ways, but the most common symptoms of osteoarthritis are:
- pain and swelling in the affected joints
- stiffness, especially if you haven’t moved for a while
- joints looking bigger than normal.
Some people with osteoarthritis can hear grating or crunching noises when moving their feet and ankles. You may also feel unsteady on your feet.
You may have an achy feeling in your feet, especially if you’ve been particularly active or worn high heels. Some people also get pain in their feet at night.
In the ankle, osteoarthritis could cause your ligaments to become weaker, which could put more strain on the cartilage. You might also find the muscles around your ankle become weaker over time, and it may feel painful to walk or put weight on your ankle.
The repair process in osteoarthritis can cause spurs to form on the edge of your bones. These are known as osteophytes (os-tee-o-fites) and change the shape of your joint. Sometimes bone and cartilage can break away and float inside the joint, which could cause more pain and swelling.
If you think you might have osteoarthritis of the foot or ankle, it’s important to visit your GP, so they can diagnose you and start treatment as soon as possible. If you’ve been diagnosed with osteoarthritis of the foot or ankle, it’s important to know that your symptoms probably won’t get worse, and they may even improve.
Are there any complications?
Osteoarthritis can sometimes cause other problems for your feet, which may get worse if the condition isn’t treated.
Hallux rigidus
If osteoarthritis in the feet is left untreated, cartilage can wear away completely. This might cause the bones of your foot to join together. When this happens in the big toe, it’s known as hallux rigidus.
This can make it more difficult to move your big toe and you may have trouble walking. Sometimes bony growths may appear on the top of your toe.
Bunions
Hallux rigidus and osteoarthritis in your big toe can cause this toe to lean towards your other toes. When this happens, it’s called a bunion or hallux valgus.
A bony lump can then form on the side of your big toe. Sometimes you might have red or swollen skin over it, and it can also cause hard skin. You might feel unsteady while standing and walking.
Corns and calluses
Corns and calluses can form on your feet in areas where they’re exposed to pressure, or the skin is repeatedly rubbed. This might be because of uncomfortable shoes. Corns are small, hard lumps of skin, and calluses are patches of thicker skin that feel rough.
Corns and calluses can sometimes be caused by other problems with your feet, such as bunions.
Managing osteoarthritis of the foot and ankle
Exercise
When you have osteoarthritis, it’s important to keep active. You might worry that exercising will make your symptoms worse, but it will improve your condition by strengthening your muscles and tendons, and nourishing the cartilage of your joints.
If you find exercising painful, it may help to take some paracetamol before you start.
There are three types of exercise you should try to do:
- Stretching exercises – which can help maintain and improve the range of movement of your joints.
- Strengthening exercises – which help to keep your muscles and joints strong and supported.
- Aerobic/fitness exercises, which just means anything that increases your heart rate.
It’s recommended that each week adults do:
- strengthening exercises on two or more days
- at least two and a half hours of moderate aerobic exercise, such as cycling or brisk walking.
Walking is a good way to stay active, and if you join a group of people doing an activity it can be more fun and help improve your health and your general wellbeing. Swimming could be a good option, because it doesn’t put weight on your toes, feet and ankles, but still helps you keep fit.
Your GP should be able to give you some advice on exercise. They may also be able to refer you to a physiotherapist, who can work with you to develop an exercise plan. As well as physiotherapy, they may also be able to refer you for hydrotherapy where exercises are done in a warm-water pool with a physiotherapist. Hydrotherapy can sometimes be called aquatic therapy.
You can find examples of exercises that could help you on our exercises for the toes, feet and ankles page.
Weight management
If you’re overweight, losing weight can really help your condition by reducing the strain you put on the joints in your feet and ankles. Increasing the amount of exercise you do and following a healthy diet are good ways to lose weight. This is great for your general health, even if you’re a healthy weight already.
There’s no specific diet that will help with osteoarthritis, but it’s important to make sure you’re getting all the nutrients you need through a healthy, balanced diet. If you’re planning to lose weight, make sure you speak to your GP first, so they can give you advice on how to lose weight safely.
Looking after your feet
It’s important to take care of your feet if you have osteoarthritis in your feet or ankles. A good footcare plan can help reduce the likelihood of you developing other problems that could make your pain worse, such as corns, calluses, or ingrown toenails.
There are a number of things you can do yourself, including:
- washing your feet every day in warm, soapy water – don’t soak your feet unless you have problems with hard skin or ingrown toenails
- drying your feet well, including in between your toes
- moisturising your feet all over, except for between your toes
- cutting your toenails regularly, cutting straight across the nail – doing it at an angle or down the sides could lead to ingrown toenails.
If you have corns or calluses, try:
- soaking your feet in warm water to soften the skin
- using a pumice stone or foot file to remove hard skin
- moisturising your feet to keep the skin soft.
It’s a good idea to get your feet checked regularly by your GP or a podiatrist. This is important if you have any problems with your feet that don’t get better after a few weeks.
Podiatry
Podiatrists , also known as chiropodists, are specialists in treating foot problems. You can either be referred to an NHS podiatrist by your GP or, in some areas, you can refer yourself.
You could also pay to see one privately. Either way, you should make sure they’re registered with the Health and Care Professionals Council (HCPC).
Your podiatrist can advise you on what footwear and treatments are most suitable for you. Treatments include:
- strapping your feet for short periods of time to limit how much you move painful joints
- providing padding or shields for your feet and toes, to reduce pressure and friction in shoes
- treating problems with your feet, such as ingrown toenails, hard skin and corns
- providing insoles or inserts to go in your shoes to support your feet.
Footwear
Getting the right footwear is very important to prevent further damage to your feet and ankles. It’s important to wear comfortable shoes, as high heels or shoes that are too small or pinch your feet can lead to problems such as hard skin or bunions.
When getting new shoes, consider the following tips:
- Wear shoes with a low heel and a wide front. This means that your feet will have enough room and your toes can spread out as you walk.
- Get your shoes professionally fitted if possible, as feet can change size. Try to get shoes with a gap of 1cm between the end of the shoe and your longest toe.
- Buy shoes in the afternoon, as your feet can swell up during the day. Trying them on in the afternoon will give you a better idea of how they fit.
- Avoid wearing shoes that don’t support your feet, like ballet pumps and flip-flops.
- Wear shoes with thick, cushioned soles to reduce the stress that walking puts on your joints.
- Try to get shoes that are deep and soft on the top, so that they’re comfortable and flexible.
- Shoes with laces or adjustable straps will help keep your foot in place, and stop your toes being pushed to the front of the shoe.
- Stiff soles can help if you have bunions.
- A light but stiff walking boot can help ankle pain.
Insoles and specialist footwear
Shoe inserts and insoles can help relieve pressure on all your joints, cushion your feet, and ease pain when you walk. You might also find that a brace or support for your ankle helps. A podiatrist can usually give you these.
Some shops sell cushioned insoles that you can put in your shoes, but you may need to see an orthotist, who specialises in splints and supports. Some companies sell insoles that mould to the shape of your foot, which will give you more support and improve your foot alignment and posture. However, you should only use these after getting advice from a healthcare professional.
If you need to wear specific footwear for work, you may find that insoles make them more comfortable. A podiatrist can give you advice.
You may be able to have a change made to your own shoes, such as a rocker being added to the affected area. Changes such as this often make walking easier.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.
Drugs
There are a number of drugs that can be used to treat osteoarthritis of the feet and ankles. However, as with all drugs, there may be some side effects. It’s a good idea to discuss them with the healthcare professionals treating you before starting any drug.
Painkillers and NSAIDs
Painkillers that you can buy over the counter, or from shops and chemists, such as paracetamol, can help with pain and stiffness. You might need to take stronger painkillers, such as compound analgesics or opioid analgesics. However, these only work for a little while and you can only get them on prescription. A common compound analgesic is co-codamol, and common opioid analgesics include morphine and tramadol.
Non-steroidal anti-inflammatory drugs (NSAIDs) can help with pain and inflammation. Ibuprofen can be bought from supermarkets and chemists, but some stronger NSAIDs, such as naproxen and celecoxib, are only available on prescription.
Some NSAIDs are also available as a cream or gel and can be rubbed over the painful areas. If you’re already taking tablets or liquid versions of NSAIDs, speak to your doctor about creams and gels first, as you might not be able to use both at the same time.
Steroid injections
Steroid injections can be given by a health professional into joints, to reduce pain and swelling in the affected area. They only last for a short amount of time, but if they work you might be able to have another one after a few months.
Other pain relief
Warmth on the affected joints has been shown to help with pain and stiffness. This can be a bath or shower in warm water, or a heat pack applied to your skin. Some packs are reusable and can be heated in the microwave.
You could use an ice pack, cold pad or pack of frozen vegetables wrapped in a damp cloth to reduce joint swelling. When applying packs to your skin, make sure you don’t put them on your bare skin, and never leave them on for longer than 20 minutes.
Another way to relieve pain is transcutaneous electrical nerve stimulation (TENS) which involves sending electrical pulses through pads attached to your skin. A physiotherapist can advise you on the different TENS machines available.
Wearing an elastic bandage on your ankle might help support it and ease pain in the joint. Another tip is to pace your activities – spreading tasks out over a day or week, rather than doing things all in one go, or until you feel tired.
Your physiotherapist may feel you’d benefit from mobilisation or manipulation. This is a treatment that involves a health professional applying controlled force to your joints with their hands.
You might also want to try complementary treatments, such as glucosamine and chondroitin supplements, to help with your symptoms. However, research shows they’re not very effective, and these treatments aren’t recommended by the NHS.
Coping with low mood and sleep problems
If your arthritis is painful, you may sometimes feel quite down. It can also be frustrating if tasks become harder. However, there are some easy ways you can look after your emotional wellbeing.
Pain clinics run sessions to help you learn how to manage your pain. They’ll usually take place in outpatient clinics, and you can be referred by whoever is treating you. They’re only normally recommended if your pain isn’t being controlled by other treatments.
There are a number of talking therapies and techniques you can learn, which can help you manage your pain and any low mood. Mindfulness and cognitive behavioural therapy (CBT) can also help with osteoarthritis.
Before bed, try having a hot bath, reading a book, or listening to the radio or a relaxation CD. If pain is waking you during the night, try taking paracetamol or another painkiller before bed. Talk to your doctor or a sleep expert for more advice.
Surgery
Surgery for the feet and ankles will only be considered if other treatments haven’t worked.
Arthroscopy and debridement
An arthroscopy involves two smaller cuts being made on either side of the ankle, or small incisions being made in the foot or around the big toe, in the case of hallux rigidus. This is a type of keyhole surgery, so the cuts are usually smaller than 1cm.
The surgeon can see the affected bone inside your foot or ankle and will be able to perform a procedure called debridement. In this, they’ll use small tools to remove any bone spurs and clean the area inside the joint.
Fusion
Fusion can be performed in your ankle, feet and toes. In this operation, the joint surfaces causing the problem are removed to allow the bones to grow together and fuse. Sometimes they are held in place with screws.
It’s not possible to undo fusion surgery and it will affect the way you walk. Because of this, it’s important to think about it carefully and talk to a surgeon before going ahead with it.
Ankle replacement
In an ankle replacement, the damaged surfaces of your ankle joint are removed and replaced with new material. A spacer made of plastic is also added between the two surfaces of the joint.
Ankle replacements will improve your pain and should improve your range of movement in the joint. However, most ankle replacements only last for around 10 years, so it’s important to talk to your surgeon, to make sure it’s the right decision for you.
Bunion surgery
There are things you can do yourself to improve any problems caused by bunions, but surgery is the only way you can get rid of them completely. In this operation, the bunion will be scraped away and your big toe straightened. Sometimes screws or staples are used to keep it in place.