What is giant cell arteritis (GCA)?
Giant cell arteritis (or GCA) is a medical condition that can cause pain and swelling in blood vessels.
Blood vessels are tubes that carry blood around the body. GCA affects arteries, which are the largest of the three types of blood vessels. Arteries take blood with oxygen in from the heart to different parts of the body.
GCA commonly affects arteries in the head and neck.
This condition can cause pain and tenderness in the soft part at the side of the head in between your eyes and ears, known as the temples. When the condition affects this part of the head it can be called temporal arteritis.
GCA can also affect other large arteries and their branches that take blood elsewhere around the body.
This condition is treatable, usually with steroid tablets. But if it’s left untreated it can be very serious and cause strokes or blindness.
GCA is one of a group of conditions called vasculitis. The word vasculitis means inflammation in blood vessels. There are different types of vasculitis, because different blood vessels can be affected.
Related information
Who gets giant cell arteritis?
GCA is very rare in people younger than 50. It’s more common in women than men, and more common in people of north European descent than in people of other races.
GCA is often linked to a condition called polymyalgia rheumatica (PMR), which causes pain and stiffness of the muscles particularly in the shoulders, neck, hips and thighs. Symptoms of PMR can be particularly bad in the mornings. Often people have both PMR and GCA.
Symptoms
People with GCA may have a number of symptoms. Most people will have some, but not all of these. The most common symptoms of GCA are:
- headaches, often with severe pain and tenderness over the temples and the scalp – it may be painful to brush your hair or to shave. Headaches from GCA can cause pain elsewhere in the head too.
- thickening or tenderness of the blood vessels at your temples
- pain in the jaw or tongue when chewing
- severe tiredness that affects your quality of life, otherwise known as fatigue
- flu-like symptoms, such as a mild fever
- sweats, during the day or night
- weight loss
- double vision
- rarely, loss of sight, which can occur suddenly. This may be partial, but it can sometimes be total. It’s usually temporary in the early stages.
If you have any changes or problems with your vision, or jaw pain while eating, you should see your doctor straight away.
If you can’t get an immediate appointment with your doctor, contact an out-of-hours doctor, or go to the accident and emergency department at the nearest hospital straight away. If left untreated these symptoms can lead to permanent sight loss or a stroke.
Serious problems can usually be avoided with prompt steroid treatment.
Less commonly, GCA can affect other large blood vessels that could lead to pain when using the arm muscles or in the calves when walking.
Rarely, if someone has had GCA or PMR for a long time, they may develop aneurysms. This is when artery walls increase in size and can bulge and become weak.
Causes
We don’t yet know fully why people develop GCA.
It’s an autoimmune condition. This is when your immune system, which is your body’s defence system that fights infections, gets confused and attacks healthy tissues in the body.
In people who have GCA, the immune system mistakenly attacks healthy arteries.
It may be that the genes you inherited from your parents made you more likely to develop GCA. However, just because someone has GCA, it doesn’t mean their children will definitely get it.
Diagnosis
A diagnosis of GCA will be made based on:
- an examination by your doctor or a specialist, and a discussion of your symptoms
- blood test results
- x-rays and scans
- a biopsy to see if there is inflammation in the walls of the temporal artery.
Should I see a specialist?
It’s very important that treatment is started straight away if GCA is suspected. A GP can start this treatment.
However, you should also be referred promptly to a specialist to confirm the diagnosis and for a treatment plan.
Depending on your symptoms, this specialist could be:
- a rheumatologist – a doctor who specialises in problems with the immune system
- an ophthalmologist – an eye specialist
- a neurologist – a doctor whose expertise is to do with the brain, nerves and spinal column
- an acute physician – a doctor within a hospital who sees medical emergencies, for example people who have turned up at an accident and emergency department.
Tests need to be performed quickly, so you’ll probably be given an urgent referral.
What tests will I have?
Blood tests
Blood tests can be carried out to check for signs of inflammation. These tests can be used to help diagnose GCA.
They will also be repeated over time to check that the inflammation is controlled. Blood tests can also be used to look for other possible causes of your symptoms.
Scans
You may be asked to have a chest x-ray to rule out other conditions.
Another test that could be suggested is a CT (computerised tomography) scan. This can help diagnose GCA and see if there are any complications. CT scans create detailed images of what is happening inside the body using many x-rays.
Your doctor may ask for an ultrasound scan of the arteries around the temples and in the armpit, to help confirm a diagnosis.
Ultrasound scans use sound waves to examine and build up pictures of the inside the body. They can show what is happening in tendons, blood vessels, joints and even organs. In the case of GCA, these scans can be helpful because they can detect swelling in blood vessels.
Temporal artery biopsy
Sometimes, a temporal artery biopsy may be carried out.
A biopsy is when a small piece of skin or tissue is taken from a part of the body and examined under a microscope. In this case it is from the temporal artery at the side of the head, but biopsies can be done elsewhere in the body too.
A local anaesthetic will be used first to numb the area.
Biopsies are carried out by a surgical doctor, but it’s a test and not a treatment. Your doctor will explain what’s involved, the risks and benefits. You’ll be asked to sign a form to say you understand what will happen, and that you’re happy to go ahead with the biopsy.
You can have this biopsy to confirm a diagnosis even if you’ve started treatment. If someone has GCA, biopsies can show how serious their condition is.
These types of investigations are not yet available in all hospitals.
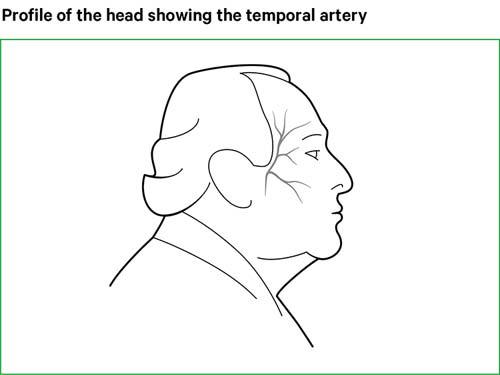
After the biopsy is carried out you’ll have a wound about 3–4 cm in length, close to the hairline. The wound will be covered with a dressing until your follow-up appointment about a week later, but you will be able to wash your hair with care. When the anaesthetic wears off you may need painkillers such as paracetamol for a while.
As with any surgical procedure, you should look out for signs of bleeding and infection – such as redness that starts to spread or a continuous discharge.
Very rarely, the procedure may lead to temporary or permanent damage to the nerves, which may result in numbness or a drooping brow. In patients who have narrowing of the arteries in the neck, known as carotid artery disease, there may be a very small risk of a stroke.
If you have any concerns about the risks, you should discuss them with your doctor beforehand.
Treatment
Steroid tablets
While there’s currently no cure for GCA, treatment with steroid tablets is very effective and usually starts to work within a few days. Prednisolone is the most commonly used steroid tablet.
Steroid tablets slow down the activity of the immune system, and reduce inflammation in blood vessels.
Because there’s a risk of sight loss or a stroke if GCA isn’t treated, it’s important to start steroid treatment straight away. If your doctor suspects you have GCA, they may prescribe a high dose of steroids before the diagnosis is confirmed.
To treat GCA, you’ll usually be given between 40 mg and 60 mg of steroid tablets every day to begin with. This dose is usually continued for three to four weeks.
If you’re well after that, and your blood tests show that your condition has improved, your doctor will start reducing the dose. During this phase, a specialist will want to see you regularly to check how you’re getting on.
If you develop visual symptoms, or pain in your jaw or tongue when eating, you may need to go to hospital urgently to be given steroids through a drip into a vein.
Usually it takes one to three years to come off steroids altogether. For most of this time, you’ll be on a low dose. It isn’t always possible to stop taking steroids completely and some people will need to be on a low dose for a long time or for all their life.
You shouldn’t stop taking your steroid tablets suddenly or alter the dose unless advised by your doctor, even if your symptoms have completely cleared up. This is because your body stops producing its own steroids, called cortisol, while you’re taking steroid tablets and needs some time to resume normal production of natural steroids when the medicine is reduced or stopped.
If the inflammation in the blood vessels returns this is called a relapse, and your steroid dose may have to be increased to deal with this. Relapse is most common within the first 18 months of treatment.
What are the side effects of steroid treatment?
As with many drugs, there are some possible side effects from steroid treatment. However, GCA is potentially a very serious condition. The benefits of taking steroids for someone with GCA, and therefore successfully treating their condition, far outweigh the risks of taking steroid tablets.
The initial high dose of steroid tablets to get the condition under control, and then the continued low dose to keep it at bay can sometimes cause the following side effects:
- changes in facial and body appearance
- facial flushing
- lack of sleep
- indigestion or stomach pain
- some weight gain
- dizziness or faintness
- difficulty concentrating
- mood changes.
Drugs called proton pump inhibitors can reduce the risk of indigestion. They do this by reducing the amount of acid produced naturally in the stomach.
If you’re on steroids for a long time, other side effects may include:
- osteoporosis – a condition that causes bones to thin and fracture more easily
- easy bruising, stretch marks, and thinning of the skin
- muscle weakness
- cataracts – a condition which causes the lens of one or both eyes to have cloudy patches
- glaucoma – a condition where the optic nerve in the eye is damaged
- diabetes – a medical condition that makes your blood sugar level to be too high
- high blood pressure.
Your regular check-ups will help to identify any side effects so that they can be treated promptly.
If you’re on steroids for longer than three months, you may need treatments to prevent thinning of the bones, including:
- calcium and vitamin D supplements
- bisphosphonates – drugs that slow down the loss of bone mass.
Because steroids reduce the activity of the immune system, you may be more likely to develop infections, and they can be more serious. For example, chickenpox and shingles can be severe in people taking steroids.
Contact your doctor if you haven’t had chickenpox, and you come into contact with someone who has either chickenpox or shingles, as you may need antiviral treatment.
Steroid cards
If you’re on steroid treatment, you should always carry a steroid card that says what dose you’re on.
If you need to see another doctor for any reason, such as if you need an operation or a hospital admission; or if you need to see a healthcare professional such as a dentist, you should tell them what dose of steroids you’re on, or show them your steroid card.
In the unlikely event that you have to be rushed to hospital in an emergency, it’s important for doctors there to know you’re on steroid treatment. Steroid treatment can affect the body’s response to an injury, and doctors will need to know you’re on steroids and give you appropriate treatment.
Steroid cards are available from most pharmacies.
Are any other drugs used to treat giant cell arteritis?
Steroids are the first-line treatment to get GCA under control and prevent any serious complications. At present, there isn’t an alternative first-line treatment available.
There are times when your doctor may suggest an additional medication to help you reduce the dose of steroids, this may happen if:
- your symptoms return, otherwise known as a relapse
- your symptoms do not improve despite steroid treatment
- you need steroid treatment for a long time.
Alternative treatments may include conventional disease-modifying anti-rheumatic drugs (DMARDs), including:
- methotrexate
- leflunomide
- azathioprine
- mycophenolate mofetil.
These drugs slow down the immune system, which can be misfiring in people who have autoimmune conditions.
There are also some newer drugs available, called biological therapies. These drugs target key cells within the immune system to stop them causing inflammation.
Biologic treatment includes medications such as tocilizumab. Tocilizumab is used mainly to treat people with relapsing large vessel vasculitis. It can also be prescribed if other treatments haven’t worked.
At times, clinical trials of possible new treatments are carried out, and you may be offered one of these new drugs as part of a scientific study. Before agreeing to take part in one of these trials, you should make sure you fully understand what it involves by talking to your doctor.
Your doctor may suggest low-strength aspirin as it helps to protect against loss of vision in GCA. You need to discuss this with your doctor to ensure it is safe for you to take aspirin.
Managing symptoms
Diet
There are no particular foods that you should avoid. However, you should eat a healthy, balanced and nutritious diet, that is low in saturated fats, sugar and salt, and contains plenty of calcium and vitamin D.
Because taking steroid tablets over the long term can increase the risk of diabetes, it’s important to have a healthy diet. Talk to your doctor if you have any concerns.
Calcium and vitamin D are important to reduce the greater risk of osteoporosis from steroid treatment.
The richest sources of calcium are:
- dairy products, such as milk, cheese and yogurt
- calcium-enriched soya milk
- fish that are eaten with the bones, for example sardines
- leafy green vegetables, beans, chick peas, some nuts and dried fruits also contain calcium.
You should have between 700 and 1,200 mg of calcium a day.
Appropriate calcium content of some common foods
| Food | Calcium content |
|---|---|
| 115 g (4 oz) whitebait (fried in flour) | 980 mg |
| 60 g (2 oz) sardines (including bones) | 260 mg |
| 0.2 litre (1/3 pint) semi-skimmed milk | 230 mg |
| 0.2 litre (1/3 pint) whole milk | 220 mg |
| 3 large slices brown or white bread | 215 mg |
| 125 g (4 1/2 oz) low-fat yogurt | 205 mg |
| 30 g (1 oz) hard cheese | 190 mg |
| 0.2 litre (1/3 pint) calcium-enriched soya milk | 180 mg |
| 125 g (4 1/2 oz) calcium-enriched soya yogurt | 150 mg |
| 115 g (4 oz) cottage cheese | 145 mg |
| 115 g (4 oz) baked beans | 60 mg |
| 115 g (4 oz) boiled cabbage | 40 mg |
Note: measures shown in ounces or pints are approximate conversions only.
Vitamin D can be obtained from some foods, especially from oily fish. Vitamin D is often added to soya milk and vegetable-based margarine. For many people, the easiest way of getting enough vitamin D is with supplements.
Vitamin D is needed to help the body absorb calcium. Vitamin D can be produced in the skin when it is exposed to sunlight during spring and summer months.
Because we can’t guarantee enough sunlight in the UK all year round, doctors recommend that we all take daily vitamin D supplements in the autumn and winter months to ensure we get enough of this important nutrient. Doctors also recommend that groups at high risk of not getting enough vitamin D take supplements all year round. This includes people:
- who don’t get out of their house or care home much and so don’t have enough exposure to sunlight
- who wear clothes which cover a lot of their skin and therefore don’t get exposure to sun
- from Afro-Caribbean and South Asian backgrounds, because darker skin is less able to process vitamin D from sunlight in the UK than paler skin.
Rest and exercise
You should keep as fit and active as you can. This helps prevent osteoporosis, and may help to avoid weight gain and muscle weakness caused by the steroids. Weight-bearing exercise, such as walking or jogging, can strengthen bones and reduce the risk of osteoporosis.
Fatigue can be a major problem for some people even when on treatment. This can be a difficult symptom to manage, and rest is important, but some people find that gradual well-paced exercise can help.
Pacing and planning activities and setting realistic, achievable goals can improve your energy levels and well-being.
If fatigue becomes a problem, it might help to have an appointment with a specialist nurse or an occupational therapist. Occupational therapists are healthcare professional who can help people improve their ability to do everyday tasks they might be struggling with because of a medical condition.
Lifestyle
Smoking can greatly damage bone health and make you more at risk of osteoporosis. Smoking can also increase the risk of having a stroke. People with GCA are already at a slightly higher risk of having a stroke than the general population, so it’s especially important not to smoke if you have GCA.
Drinking too much alcohol is bad for bone health, because it makes it harder for the body to use calcium to make bones strong.
Maureen’s story

I will always be incredibly grateful to the doctor I saw one night at accident and emergency who spotted the symptoms of giant cell arteritis and possibly saved my sight.
I had been to a GP surgery three days before because I was having these real bad pains in my head. I was given a date for an ultrasound scan to try to get to the bottom of what was going on, but this appointment was not for another eight weeks.
I was at home in the evening three days later and my symptoms got much worse. I had these lumps in my temple, and then all of a sudden I couldn’t open my jaw. I had real pain in my head.
My partner Brian said ‘Right, we’re going to A&E’. I am so glad he was insistent and didn’t take any chances. We went straight to the accident and emergency department at the local hospital.
I saw a lovely doctor. She heard my symptoms and gave me 60 mg of steroid tablets. She said to me ‘Take them immediately’.
I asked her what the panic was and she said ‘I think you have giant cell arteritis, and it can affect your eyesight’.
I saw a specialist a couple of days later, and he confirmed it was giant cell arteritis.
After two months of steroid treatment, I was told it had cleared up. I have since developed large vessel vasculitis and I’ve had to go back on the steroid tablets. I’ve not got any symptoms for that.
I am just so grateful that the doctor at A&E that evening spotted the symptoms of giant cell arteritis and knew what to do.