Guidance on clinical audit process
Clinical audits are a way in which to measure and improve the quality of clinical care. This impact toolkit provides suggestions on specific musculoskeletal topic areas for audit – each section includes relevant standards and guidelines to audit performance against and actions to be taken in order to implement the audit.
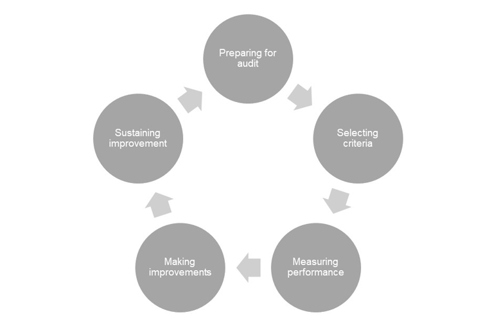
The diagram below gives an overview of the audit cycle.
Resources on running a high quality clinical audit – including details on the methods, tools, techniques and activities at each stage of a clinical audit – can be found at:
- Criteria and Indicators of Best Practice in Clinical Audit – published by the Healthcare Quality Improvement Partnership (HQIP)
- Principles for Best Practice in Clinical Audit – endorsed by NICE and the Healthcare Commission
The Quality and Outcomes Framework (QOF)
What is the QOF?
The Quality and Outcomes Framework (QOF) was developed for the GP contract in 2004. It is a voluntary scheme for practices throughout the UK which provides financial incentives to encourage high-quality care.
The QOF is divided into four different domains:
- clinical
- public health
- quality and productivity
- patient experience.
Every domain has a set of indicators relating to quality standards that can be achieved within that domain grouped under topic-based headings, such as atrial fibrillation or hypertension. Data required should be available from practice clinical systems. In recent years, musculoskeletal indicators have been added to the clinical domain including indicators for rheumatoid arthritis and osteoporosis.
All achievement against quality indicators converts to points. Each point has a monetary value and therefore practices strive to achieve as many quality points as possible to maximise payments. Payments may be adjusted according to the prevalence of the condition in a practice, list size and also factors such as deprivation and rurality. Practice achievement against the QOF is published annually.
Further details can be found at NICE: About the Quality and Outcomes Framework (QOF).
Gout
One of the most common causes of inflamed joints, gout affects approximately one in 100 adults in the UK. In contrast to other causes of inflamed joints such as rheumatoid arthritis, which are usually treated by hospital specialists, gout is largely managed in primary care.
Guidelines
The British Society for Rheumatology (BSR) and British Health Professionals in Rheumatology (BHPR) guidelines for the management of gout:
These guidelines are under revision and updated versions are due for publication in 2016.
Guidelines written by Dr Louise Warburton, president of the Primary Care Rheumatology Society, which appeared in GP Magazine, in November 2012.
Clinical knowledge summary
National Institute for Health and Care Excellence (NICE) clinical knowledge summary for the management of gout.
Audit criteria
All patients with gout should have:
- screening for co-morbid disorders (BP, HbA1c and fasting lipids) recorded within the past five years
- documented advice on lifestyle modification (weight reduction, alcohol intake and dietary adjustment)
- been signposted to information about their condition and this should be documented in their notes.
All patients with > one documented attack of gout in the past 12 months should be taking (or have been offered) a uric acid-lowering drug.
All patients with gout should have a medication review performed in the past year.
Patients with gout should not be prescribed a thiazide or loop diuretic unless there is a documented rationale for doing so.
All patients on uric acid-lowering therapy (BNF section 10.1.4) should be treated to target levels of reduction in plasma urate levels (360μmol/L or 6mg/dl).
Other suggested audits
Search for patients on uric acid-lowering therapies (BNF section 10.1.4)
- Do they have gout documented as a diagnostic code?
- Are they being treated to target levels of reduction in plasma urate levels (360μmol/L or 6mg/dl)?
Resources
Read code: C34 Gout
Low back pain
Low back pain is a common disorder, affecting around one-third of the UK adult population each year. Around 20% of people with low back pain (that is one in 15 of the population) will consult their GP.
Standards
National Institute for Health and Care Excellence (NICE) [CG88] guidance for early management of non-specific low back pain. This guidance is being revised and an updated version is due to be published in November 2016.
Audit criteria
Assessment of all patients with low back pain and radicular pain includes assessment of the risk of developing persistent disability:
- severity of pain
- the impact of the back pain
- the risk of persistent disability.
Screening tool
STarT Back screening tool for assessment of risk of developing persistent disability. This tool enables healthcare professionals to provide patients with targeted treatment. Keele University runs a course to teach healthcare professionals how to use the screening tool.
Resources
Read codes for low back pain:
- N140-1
- N142 Low back pain
- N142-1
- N142-3
- N142-4
- N143 Sciatica
- N143-1
- N145 Backache unspecified
- N145-1
- N145-2
- N1402
- N1420 Pain in lumbar spine
- S57z Back sprain NOS
- S57z0 Pulled back muscle
- 16C2 Backache
- 16C3 Backache with radiation
- 16C5 C/O low back pain
- 16C6 Back pain no radiation
- 16C8 Exacerbation of backache
- 16C9 Chronic low back pain
- 16CA 16CZ Backache symptom
Osteoarthritis
Osteoarthritis is a clinical syndrome of joint pain accompanied by varying degrees of functional limitation and reduced quality of life. It is the most common form of arthritis and one of the leading causes of pain and disability worldwide. Knees, hips and small hand joints are most commonly affected.
Standards
National Institute for Health and Care Excellence (NICE) guidance [CG177]: Osteoarthritis: Care and management in adults.
Clinical knowledge summary
NICE clinical knowledge summary for the management of osteoarthritis.
Resources
Read codes:
- N05 Osteoarthritis and allied disorders
- N09 Other and unspecified joint disorders
Osteoporosis
Osteoporosis is a disease characterised by low bone mass and structural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture. Osteoporosis leads to nearly nine million fractures annually worldwide.
Pathway
National Institute for Health and Care Excellence (NICE) pathway for diagnosis, treatment and care of people with osteoporosis.
Clinical knowledge summary
NICE clinical knowledge summary: Osteoporosis – prevention of fragility fractures.
Audit criteria
Patients at increased risk of fragility fracture should have their fracture risk formally assessed with a validated tool such as NICE guidance on Osteoporosis: assessing the risk of fragility fractures.
Risk factors include:
- prior fragility fracture
- known low bone mineral density (BMD)
- body mass index (BMI) <19kg/m2
- parental history of hip fracture
- glucocorticoid use (any dose for ≥ three months)
- alcohol use ≥ three units daily
- rheumatoid arthritis
- housebound
- smoking
- secondary causes of osteoporosis – these include:
- inflammatory bowel disease (e.g. Crohn's disease)
- malabsorption (e.g. coeliac disease)
- cystic fibrosis
- hyperthyroidism
- hyperparathyroidism
- vitamin D insufficiency
- immobilisation (e.g. resulting from CVA or Parkinson's disease)
- chronic obstructive pulmonary disease
- diabetes melitus type 1
- chronic renal and hepatic disease.
Other audit and case-finding projects can be found at Osteoporosis Resources for Primary Care. This piece of work is the result of a joint initiative between the Royal College of General Practitioners and the National Osteoporosis Society. The aim of the project was to equip GPs, practice nurses and other members of the practice team with relevant information about osteoporosis in light of the inclusion of the condition in the Quality and Outcomes Framework.
Resources
Osteoporosis Case Finding in Primary Care (Patient.co.uk) – for Read codes and case-finding information.
FRAX – 10-year fragility fracture risk, adjusted for RA.
QFracture-2012 – 10-year fragility fracture risk, adjusted for RA.
Polymyalgia rheumatica
Polymyalgia rheumatica (PMR) is the most common inflammatory rheumatic disease in the elderly and is one of the biggest indications for long-term steroid therapy. There are difficulties in diagnosis, with heterogeneity in presentation, response to steroids and disease course.
Standards
The British Society for Rheumatology (BSR) and the British Health Professionals in Rheumatology (BHPR) guidelines for the management of polymyalgia rheumatica.
Clinical knowledge summary
National Institute for Health and Care Excellence (NICE) clinical knowledge summary for the management of polymyalgia rheumatica.
Audit criteria
Diagnosis
All patients with PMR:
- have been diagnosed using core inclusion and exclusion criteria (see standards above for these criteria), followed by assessment of the response to a standardised dose of steroid
- have documented in their medical record the minimum data set (the core clinical inclusion and any exclusion criteria and laboratory investigations before commencement of steroid therapy) which forms the basis for the diagnosis.
- should be signposted to information about their condition and this should be documented in their notes.
Treatment
All patients with PMR:
- without signs or symptoms of temporal arteritis or giant cell arteritis are treated with low-dose steroid therapy according to BSR and BHPR guidelines with gradually tailored tapering according to symptoms and inflammatory markers
- being treated with steroid therapy should be issued with a steroid treatment card.
Monitoring
All patients being treated for PMR:
- have laboratory monitoring every 3 months (full blood count, ESR/CRP, urea and electrolytes, glucose)
- have assessment of fracture risk and be offered bone protection as appropriate when initiating steroids, to prevent the complications of osteoporosis
- are monitored for response to treatment, disease activity, complications of disease (including symptoms of giant cell arteritis e.g. headaches, jaw claudication and large-vessel disease), atypical features or those suggesting an alternative diagnosis, adverse effects and complications of therapy according to this follow-up schedule: Weeks 0, 1–3, 6, Months 3, 6, 9, 12 in first year (with extra visits for relapses or adverse events).
Resources
Read code: N20 Polymyalgia rheumatica.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is an inflammatory disease which largely affects synovial joints. RA typically affects the small joints of the hands and the feet, and usually both sides equally and symmetrically, although any synovial joint can be affected. It is a systemic disease and so can affect the whole body, including the heart, lungs and eyes. There are approximately 400,000 people with RA in the UK. The incidence of the condition is low, with around 1.5 men and 3.6 women developing RA per 10,000 people per year. This translates into approximately 12,000 people developing RA per year in the UK.
Standards
National Institute for Health and Care Excellence (NICE) guidelines [CG79] Rheumatoid arthritis in adults: management.
The British Society for Rheumatology (BSR) and British Health Professionals in Rheumatology (BHPR) guideline for the management of rheumatoid arthritis (after two years).
Quality and Outcomes Framework (QOF) menu indicators for RA (NM55, NM56, NM57, NM58):
- The practice can produce a register of all patients aged 16 years and over with rheumatoid arthritis.
- the percentage of patients with rheumatoid arthritis aged 30–84 years who have had a cardiovascular risk assessment using a CVD risk assessment tool adjusted for RA in the preceding 15 months
- the percentage of patients aged 50–90 years with rheumatoid arthritis who have had an assessment of fracture risk using a risk assessment tool adjusted for RA in the preceding 27 months
- the percentage of patients with rheumatoid arthritis who have had a face-to-face annual review in the preceding 15 months.
Audit criteria
Audit performance against NICE CG79 using the audit support tool developed to support the implementation of NICE guidance. The aim is to help NHS organisations with a baseline assessment and to assist with the audit process, thereby helping to ensure that practice is in line with the NICE recommendations.
People with autoimmune diseases such as RA and also those receiving immunosuppressive treatments for their disease are at increased risk of respiratory infections and related complications. Therefore all patients with RA should be offered immunisation against influenza and pneumococcus.
Patients with RA have an increased risk of cardiovascular events, similar to patients with type II diabetes. Remember that patients with high inflammatory markers carry an increased risk of cardiovascular disease. Many deaths in RA are caused by cardiovascular events driven by inflammatory components of their disease. Therefore, as well as assessment of CVD risk using a CVD risk assessment tool adjusted for RA, all patients with RA should have the following documented in their patient notes and be offered appropriate interventions to reduce their CVD risk:
- measurement of BP
- measurement of fasting lipids
- measurement of glucose
- weight and BMI
- waist measurement
- advice around physical activity and exercise
- smoking cessation advice.
Patients with RA have a high incidence of depression. Therefore all patients with RA should be screened for depression using a validated tool e.g. ultra-short screening tool, Patient Health Questionnaire (PHQ-9) or the Hospital Anxiety and Depression Scale (HADS).
Resources
Read code: N040 rheumatoid arthritis.
FRAX: WHO fracture risk assessment tool This risk assessment tool is adjusted for RA.
QFracture-2012 10-year fragility fracture risk, adjusted for RA.
QRISK2-2012 cardiovascular disease risk calculator: This CVD risk assessment tool is adjusted for RA to work out the risk of having a heart attack or stroke over the next 10 years. It is suitable for people who do not already have a diagnosis of heart disease or stroke.
NICE guidelines [CG127] Hypertension in adults: diagnosis and management.
NICE guidelines [CG181] Cardiovascular disease: risk assessment and reduction, including lipid modification.
Corticosteroids
Corticosteroids and immunosuppression
Standards
Patients on long-term corticosteroid treatment are considered immunosuppressed and should be offered a seasonal influenza vaccine and pneumococcal vaccine. See the British National Formulary (BNF) section 14.4 Vaccines and antisera. (Log-in required).
Audit criteria
- All adult patients on 20mg or more a day or children on 1mg/kg/day or more for longer than one month should be offered pneumococcal and seasonal influenza vaccination.
Search strategy
- Search for patients on systemic corticosteroids (BNF section 10.1.2) on repeat/automatic prescriptions.
- Refine search to adults on 20mg or more a day or children on 1mg/kg/day or more for longer than 1 month.
- Refine your search for influenza (65E) and pneumococcal (6572) vaccinations.
- Those patients who have not been vaccinated should be offered pneumonia and seasonal influenza vaccination.
Corticosteroids and osteoporosis risk
Standards
BNF section 6.6 – corticosteroid-induced osteoporosis.
Glucocorticoid-induced osteoporosis: a concise guide to prevention and treatment. This was published in 2002 by The Bone and Tooth Society, National Osteoporosis Society and Royal College of Physicians.
Audit criteria
All patients taking (or who are likely to take) >5mg a day of prednisolone (or equivalent) for over three months
- should be assessed for their risk of fragility fracture
- should have the following documented in their notes:
- dietary advice (especially adequate calcium and vitamin D)
- advice regarding regular weight-bearing exercise
- advice regarding maintenance of body weight
- smoking status and appropriate intervention
- alcohol use and appropriate intervention
- assessment of falls risk and advice if appropriate.
Search strategy
- Search for patients on systemic corticosteroids (BNF section 10.1.2) on repeat/automatic prescriptions.
- Follow algorithm to aid decisions on whether to investigate and/or treat these patients (see section BNF section 6.6.2) for their fragility fracture risk.
Corticosteroids and adrenal suppression
During prolonged therapy with corticosteroids adrenal atrophy develops and can persist for years after stopping. This places patients at high risk of adverse sequelae including acute adrenal insufficiency, hypotension or death.
Standards
BNF 6.3.2 Glucocorticoid therapy: cautions and contra-indications of corticosteroids.
Audit criteria
All patients taking (or who are likely to take) >5mg a day of prednisolone (or equivalent) for over three months should be issued with a Steroid Treatment Card which gives guidance on minimising risk and provides details of prescriber, drug, dosage and duration of treatment.
Disease-modifying anti-rheumatic drugs (DMARDs)
Standards
The British Society for Rheumatology (BSR) and British Health Professionals in Rheumatology (BHPR) guidelines for disease-modifying anti-rheumatic drug (DMARD) therapy, in consultation with the British Association of Dermatologists.
British National Formulary section 10.1.3 Drugs that suppress the rheumatic disease process.
National Institute for Health and Care Excellence (NICE) clinical knowledge summary for DMARDs.
Assessing, managing and monitoring biologic therapies for inflammatory arthritis: guidance for rheumatology practitioners from the Royal College of Nursing.
Audit criteria
All patients on DMARDs (whether hospital- or GP-prescribed) should have the drug documented on their current medication to alert prescribers to possible drug interactions.
All patients on DMARDs should have ‘high-risk drug monitoring’ coded as an active problem in their medical records.
All patients on DMARDs should be managed according to local shared care guidelines (if medication prescribed in primary care) and be in possession of a disease-monitoring book.
All patients on DMARDs should have regular blood monitoring which conforms with BSR/BHPR guidance.
All patients on DMARDs should be offered pneumonia and seasonal influenza vaccination.
Patients on DMARDs should be signposted to information and this should be documented in their notes.
Resources
Read code: 66P high-risk drug monitoring.
Read code: 65E (influenza) and 6572 (pneumococcal) vaccinations.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Standards
There are long-standing and well recognised gastrointestinal and renal safety concerns with all non-steroidal anti-inflammatory drugs (NSAIDs). There is also an increased risk of cardiovascular events with many NSAIDs, including COX-2 inhibitors and some traditional NSAIDs. The Medicines and Healthcare products Regulatory Agency (MHRA) recommends that the lowest effective dose of any NSAID should be prescribed for the shortest time necessary for control of symptoms.
The National Institute for Health and Care Excellence (NICE) has produced advice [KTT13] on prescribing NSAIDs based on the evidence base.
Drug safety update
The MHRA issued a drug safety update in June 2013, entitled Dicolfenac: new contraindications and warnings.
Audit criteria
- All patients prescribed NSAIDs should have a review of the appropriateness of the prescription on a routine basis, especially in people who are at higher risk of both gastrointestinal and cardiovascular morbidity and mortality (for example, older people).
- All patients over 45 years old prescribed NSAIDs should be co-prescribed a proton pump inhibitor in accordance with NICE clinical guidelines.
- All patients prescribed NSAIDs on a repeat/automatic prescription should have an annual record of their renal function (eGFR and creatinine).
- All patients prescribed NSAIDs on a repeat/automatic prescription should have an annual record of their blood pressure.
Resources
Search for patients on repeat/automatic NSAIDs (BNF 10.1.1).
Hospital-prescribed drugs
Cytokine-modulating drugs should be initiated and prescribed under specialist supervision, so prescribing GPs may be unaware that patients are taking these drugs. A strategy is required to case-find patients who are prescribed these drugs in specialist care to avoid harm from medication interactions and also to raise awareness of possible immunosuppression, the increased risk of rapid spread of infection and to avoid administration of live vaccines.
The National Institute for Health and Care Excellence (NICE) has a compilation of advice, information and guidance relating to cytokine-modulating drugs on its website.
Audit criteria
All patients prescribed medication by a hospital or specialist team should have this medication documented on their GP medication list as well as the indication and information on the prescribing team in their GP records.
Search strategy
- Search for patients coded as: rheumatoid arthritis (N040), ankylosing spondylitis (N100), psoriatic arthritis (M160), juvenile idiopathic arthritis, systemic lupus erythematosus (N000z).
- Review current medication list on these patients to see if they are documented to be prescribed cytokine-modulating drugs (BNF section 10.1.3: cytokine modulators).
- Review recent letters from their rheumatology teams to confirm which medication they are taking.
- Add any hospital-prescribed medication to the patient's current medication list. Consider ways to do this that will prevent accidental issuing/dispensing of medications e.g. 'Hospital prescription for information only. Do not issue, do not dispense. Quantity 1' .
- Consider adding Read code 66P (high-risk drug monitoring) as an active problem in patients' notes.
Investigations for musculoskeletal problems
Investigation of musculoskeletal (MSK) problems can present challenges to clinicians. There is a lack of definitive tests available and skills are needed to interpret results. There is also the potential to do harm to patients, both in terms of physical harm, for example from ionising radiation, but also by reinforcing worries about physical damage to tissues which can then pose a barrier to improvements.
The investigation of MSK complaints, therefore, need to be carried out carefully and astutely. Relevant and timely follow-ups can be very positive.
Serology
Review 20 patients you have seen in the last year who have had rheumatology serology tests (eg rheumatoid factor, anti-CCP, HLA-B27, ANA/ANF).
Were these patients subsequently referred to see a rheumatologist?
- How much information did the tests add to the clinical picture?
- Did they affect your management of the patient?
X-rays
Consider performing a retrospective review of patients who have had x-rays for knee pain in the past year:
- Was your request in keeping with Royal College of Radiologists (RCR) iRefer guidelines? These can be accessed by all healthcare professionals via e-Learning for Healthcare (e-LfH).
- How will this change your approach in future?
Consider performing a retrospective review of patients who have had x-rays for back pain in the past year:
- Was your request in keeping with RCR guidelines?
- How will this change your approach in future?
Magnetic Resonance Imaging (MRI)
Standards
RCR iRefer guidelines. Consider performing a retrospective review of patients who have had MRI scans for knee injuries (read code for MRI scan: 56N91):
- Was your request in keeping with RCR guidelines?
- Did your history and examination findings correlate with the MRI report?
- How will this change your approach in future?
Consider performing a retrospective review of patients who have had MRI for back or neck pain (with or without radiculopathy):
- Was your request in keeping with RCR guidelines?
- Did your history and examination findings correlate with the MRI report?
- How will this change your approach in future? How confident do you feel about diagnosing a prolapsed disc without an MRI scan?