What is osteomalacia?
Osteomalacia is the name of a condition where bones become soft and weak. This means they can bend and break more easily than normal.
The most common cause is not having enough vitamin D.
Rickets is the name of a similar condition that affects children.
Why do bones become soft?
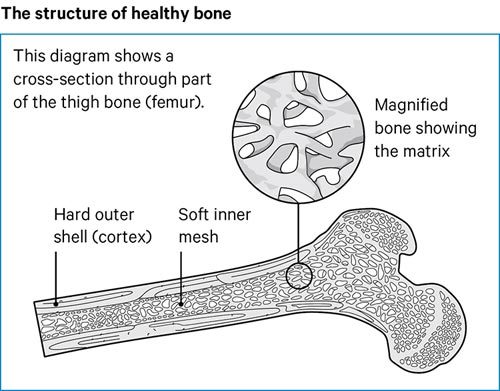
To understand osteomalacia, it’s worth looking at what happens inside bones.
Bone is a living tissue. Old bone cells are continuously being removed and replaced with new cells. This is called bone turnover.
Bone has a hard outer shell, called the cortex.
Inside the bone there’s a softer and lighter structure, called the matrix. It has a structure a bit like a mesh or honeycomb.
To protect the inner part of bone, layers of calcium and phosphorus are laid down on top of it to form the outer shell. The strength of the bone depends on how much of these minerals is laid down.
Vitamin D controls levels of calcium and phosphorus in your body. For example, vitamin D will help your body take calcium out of food so it can be used to make bones strong.
If you don’t have enough vitamin D, calcium or phosphorous, bones will become soft and weak.
What are the symptoms of osteomalacia?
Often in the early stages there aren’t any symptoms.
However, as the condition progresses, osteomalacia can cause:
- pain felt in the bones and joints
- muscle pain and weakness, particularly following exercise
- bones that break more easily, particularly those in the hips, lower back and feet
- difficulty walking and a change in how you walk – possibly with a waddle
- muscle cramps
- pins and needles in the hands and feet because of low calcium levels.
Bone pain is felt most often in the legs, groin, upper thighs and knees. It’s sometimes felt in the feet when you stand, walk or run.
Sitting or lying down to rest often eases the pain. Sometimes a slight knock on a bone such as the shin will feel very painful. As the condition gets worse, pain can be felt all over the body and simple movements can hurt.
Muscles may become weak or feel stiff. The weakness tends to affect muscles in the thighs, shoulders and main part of the body – the trunk. This can make it difficult to climb stairs, get up from a chair without using the arms for support and, in very severe cases, get out of bed.
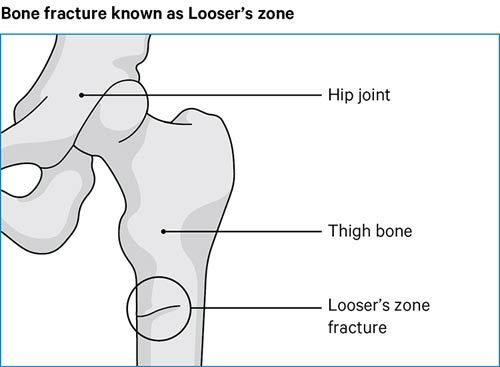
Partial fractures linked with osteomalacia are called Looser’s zones (see diagram below) which can be very painful and make walking difficult. Occasionally, these cracks can lead to full breaks, known as complete fractures.
Bones can break more easily from falls or simple knocks that wouldn’t normally cause a broken bone. This is often how people find out they have osteomalacia.
Who gets osteomalacia?
Anyone who doesn’t have enough vitamin D is at risk developing osteomalacia.
The best source of vitamin D is sunshine on skin. Some people don’t get enough sunshine on their skin and this increases their risk.
People who are commonly affected in this way include those who:
- are too frail or ill to go outside
- wear clothing that covers a lot of their skin. For example, women who wear clothes that cover all their skin for religious reasons, such as a burka, might not expose their skin to enough sunlight
- have dark skin, which is not as good as paler skin at processing vitamin D from sunlight. This can include people from Middle Eastern, Afro-Caribbean and South Asian communities.
Pregnant and breastfeeding women, and children need high levels of vitamin D, and sometimes people in these groups might not be getting enough.
In rarer cases, the following can make people more at risk of osteomalacia:
- kidney failure
- liver diseases
- some medications, such as epilepsy tablets
- untreated coeliac disease
- if you have had surgery on your stomach.
If any of the above applies to you, you may need extra protection against osteomalacia. It’s important to talk to your doctor about this.
Getting enough vitamin D
The body makes its own vitamin D when bare skin is exposed to sunlight.
From April to the end of September, most people living in the UK will be able to get the vitamin D they need from sunlight.
People with white skin will usually need 10 to 15 minutes of midday sunshine, two to three times a week. This means sunshine on bare skin, such as the arms, legs and face – without sun cream or clothes on those parts of the body.
People with darker skin may need a bit more time in the sunshine.
While it is very important for bone health to get sunshine like this, you need to be careful not to get sunburned. If your skin is feeling hot or going red you will need to cover up or go into the shade.
If you have further questions about getting the right amount of sunshine, talk to a doctor or pharmacist.
Vitamin D is present in small amount in some foods, such as:
- oily fish
- red meat
- egg yolk
- fortified breakfast cereals
- fortified butters and spreads.
Eating foods high in vitamin D can help, but you won’t be able to get all the vitamin D you need from food alone.
In the UK we can’t rely on sunshine all year round to give us the vitamin D we need.
Because of this, the Department of Health recommends that everyone should take vitamin D supplements from the beginning of October to the end of March.
Some people are advised to take vitamin D supplements all year round. This includes people who:
- don’t go outside much
- wear clothes that cover a lot of their skin
- have dark skin.
Calcium and bone health
Calcium is needed to make bones strong and a lack of calcium can cause osteomalacia. Because it’s fairly easy for most people to get enough calcium from their diet, a lack of calcium is not a common sole cause of osteomalacia. But it’s still worth knowing which foods are high in this important nutrient.
Good sources of calcium include:
- milk, cheese and other dairy products
- green leafy vegetables, like broccoli, cabbage and okra, but not spinach
- soya beans
- tofu
- soya drinks added with calcium
- nuts
- bread and anything made with fortified flour
- fish where you eat the bones – such as sardines.
The calcium from food can only get absorbed when you have enough vitamin D in the body.
How is osteomalacia likely to affect me?
Most people with osteomalacia will recover with treatment. However, it can take months for bones to recover and for muscles to become strong again.
A late diagnosis can make recovery more difficult, especially if bones have fractured.
How is osteomalacia diagnosed?
Because it doesn’t always cause symptoms, it’s common for people to have osteomalacia for two or three years before it’s diagnosed.
What tests are there?
A simple blood test is all that’s needed to make the diagnosis – the levels of calcium, phosphorus and vitamin D are easily measured.
Blood tests for the following also help to make the diagnosis:
- Alkaline phosphatase, which is a substance made by the cells that make bone. This is at a raised level in people who have osteomalacia.
- Parathyroid hormone, produced by the parathyroid gland, is raised as part of the body’s reaction to low vitamin D levels.
Blood tests will be able to rule out some of the rarer causes of the condition, while an x-ray may show any cracks or fractures in the bones.
What treatments are there for osteomalacia?
Treatment will cure osteomalacia in most cases, but easing bone pain, muscle weakness and cramps may take several months.
If it’s caused by a lack of vitamin D, you will probably need to take vitamin D supplements every day. Taking calcium supplements every day too may speed up bone healing.
You may need to take vitamin D supplements over a long period of time and if you stop taking them, the condition may return.
Once you begin treatment for the condition any cracks in your bones will heal normally, though you may need painkillers in the meantime. You should avoid intensive exercise until the cracks have healed.
People with kidney failure or inherited forms of osteomalacia often need lifelong support from their doctor. They’ll need to be monitored regularly in a hospital. They usually need special forms of vitamin D such as calcitriol tablets.
Self-help and daily living
There are many things you can do to promote healthy bones, such as:
- having a diet rich in vitamin D and calcium
- getting a healthy amount of sunshine
- only drinking alcohol in moderation
- not smoking
- exercising regularly
- maintaining a healthy weight.
Exercise
Exercise helps to strengthen bones and muscles, especially weight-bearing exercise.
Exercises that place some resistance against muscles makes them stronger. This can include walking, running or lifting weights.
You should avoid intensive exercise while any fractures or cracks in the bones are healing.
For more information about exercise, talk to a doctor or physiotherapist.