Purpose of the report
Versus Arthritis has worked hard for musculoskeletal conditions – and the chronic pain they cause – to be recognised as a public health issue.
Chronic pain has been called an invisible condition. Although often devastating to the millions who have it and being one of the biggest causes of disability in the UK, to others it cannot be seen.
Public health decisions must be informed by robust, reliable data. So Versus Arthritis funded the Health Survey for England 2017 to repeat the same questions about chronic pain that had been asked six years earlier.
In this report, we set out key findings from the survey (initially analysed by Public Health England) and a series of recommendations which call for a fundamental re-think in how we support people with chronic pain through far-reaching solutions.
Download the full ‘Chronic pain in England: Unseen, Unequal, Unfair report’ (PDF, 5.8 MB).
Download the printer friendly version of the report here (PDF, 11 MB).
What do we mean by chronic pain?
Chronic pain usually refers to persistent or recurrent pain that has gone on for more than three months. In this report, we define chronic pain as pain or discomfort that troubled a participant either constantly or intermittently for more than three months (12 weeks).
High-impact chronic pain is chronic pain which is severe and where people are unable to carry out their daily activities.
Some chronic pain is caused by underlying inflammation or damage to the body’s tissues. In arthritis there is inflammation or damage in the joints and neuropathic pain can be caused by damage or inflammation in the nerves.
Other conditions, such as fibromyalgia, are a type of chronic primary pain. These are conditions in their own right where the chronic pain is complex and associated with many other symptoms, rather than being due to underlying disease or damage in the joints or nerves.
The findings are stark
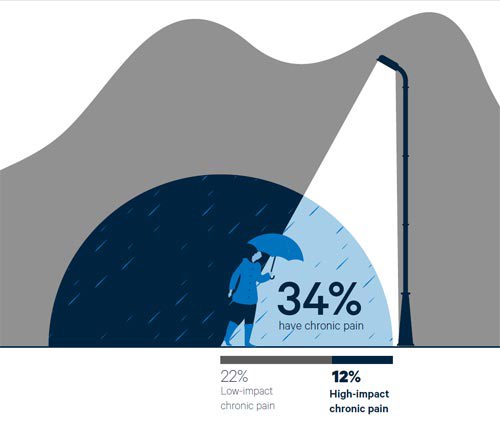
- Around 15.5 million people in England (34% of the population) have chronic pain.
- Approximately 5.5 million people (12% of the population) have high-impact chronic pain and struggle to take part in daily activities.
- 10 million people (22% of the population) have low-impact chronic pain.
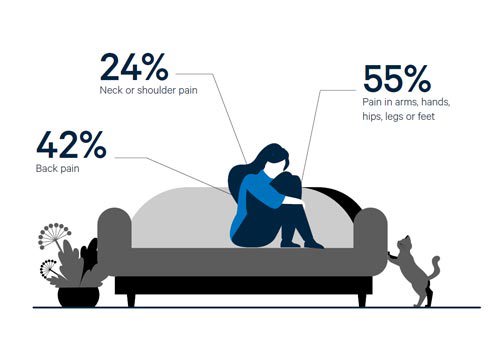
Musculoskeletal conditions such as osteoarthritis, back and neck pain are the commonest cause of chronic pain.
- About 8 in every 10 people (84%) with chronic pain report that at least some of their chronic pain is in the neck or shoulder, back, limbs or extremities – all sites where pain is most likely to be musculoskeletal (25% neck or shoulder pain, 42% back pain, and 55% pain in arms, hands, hips, legs, or feet).
Unequal and Unfair
The same health inequalities that are seen in many long-term conditions are also seen in chronic pain. Adverse social and psychological experiences increase people’s risk of developing chronic pain. Groups that in our society experience greater life stress, disadvantage and discrimination are more likely to have chronic pain.
- Chronic pain is linked to deprivation. People who experience high-impact chronic pain are twice as likely to live in the most deprived areas (30%) compared to the least deprived areas (15%).
- Chronic pain more prevalent in women than men. Not only are women more likely to have chronic pain than men of the same age, but women also report more high-impact pain than men. 14% of women have high-impact chronic pain compared to 9% of men.
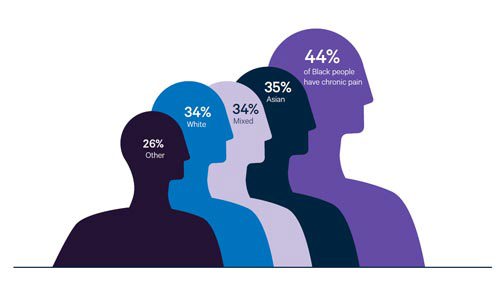
- Chronic pain disproportionately affects some minority ethnic groups. Black people are more likely to have chronic pain than people of other ethnic backgrounds. 44% of Black people have chronic pain, compared with 34% of white, 35% Asian, 34% mixed/multiple ethnicities, and 26% any other ethnic background.
- A rise in chronic pain in young adults. High impact chronic pain appears to have become more common among young people with chronic pain, rising from 21% to 32% between 2011 and 2017.
What needs to happen?
We need to see a fundamental re-think in how we support people with chronic pain through far-reaching solutions. The approach must be holistic, comprehensive and integrated across our health and care systems and public health, at a national - and fundamentally - at a local level.
This report makes a series of recommendations to leaders of local health and care service and public health in the following areas:
- Identifying those who have chronic pain
- Assessing and meeting people’s needs
- Reducing health inequalities
- Prevention of risk factors for ill health
- Supporting those who are able to work
- Improved coordination and monitoring of progress.
Download the full ‘Chronic pain in England: Unseen, Uneuqal, Unfair report’ (PDF, 5.8 MB).
Download the printer friendly version of the report here (PDF, 11 MB).
Victoria’s story
 “I’m Victoria, I’ve lived with chronic pain for over eight years.”
“I’m Victoria, I’ve lived with chronic pain for over eight years.”
Living life with constant pain is physically and mentally exhausting.
It all started after I suffered whiplash in a car accident in 2012. The pain never went away, and things only got worse over the years that followed.
At first, I was hesitant to take medication, yet I was also fed up with being in pain and not being able to pursue my normal way of life, which has always been very active. So, I agreed to try medication, hoping it would improve things. I went through many different tests and therapies, but still had no answers.
“The pain slowly increased over the years until I had it every single day, all over my body.”
I couldn’t stand up or move without being in pain and it was filling my every waking hour. On top of this, I was told by several doctors that I probably wouldn’t be able to conceive a child due to the level of stress my body was under.
After more failed medical treatment, my desperation drove me to another physiotherapist – this time, a good friend of mine – who has excellent understanding of pain management.
Over a lengthy period of physiotherapy sessions and multiple discussions about pain science, I had a breakthrough.
“I learned that there are a huge range of factors that can influence pain, such as emotions, beliefs and relationships.”
I also learned that understanding why you are in pain and re-framing how you think about it can change how you experience it.
Pacing my activity was key to my improvement yet once I conquered this, it enabled me to think about reducing my medication.
Shortly after giving birth, a second episode of chronic pain occurred in the form of pelvic pain. I had to re-educate myself about chronic pain and pain science to understand why I was in pain again.
It was really hard for me to accept that I was back to being a chronic pain sufferer. However, because I was more informed about chronic pain and I was able to receive support much earlier, my pain levels have been much lower. I won’t give up hope.
Sharon’s story
 “I’m Sharon, I’m 51 and living in chronic pain due to hypermobility syndrome and fibromyalgia. “
“I’m Sharon, I’m 51 and living in chronic pain due to hypermobility syndrome and fibromyalgia. “
I worked as a nurse before I was diagnosed. It was very high intensity, with long shifts and often I didn’t have a chance to look after myself. I started getting cysts all over my body and I had nine surgeries over an 18-month period.
I never recovered after the final surgery in 2013. I ran out of energy as soon as I got out of bed and everything hurt. My body was just a ball of pain.
“My doctor said it could be fibromyalgia, which was later confirmed by the rheumatologist.”
I was told that I might improve and be able to go back to work, but that hasn’t happened for me. Things just got worse; and the pain has made me miserable.
Living with pain means your whole way of life changes. I was looking after other people all the time, then I went to wetting myself because I couldn’t get to the toilet, not being able to make myself a meal, having to crawl up the stairs because I couldn’t walk for the pain.
“The pain is constant and nothing ever relieves it completely.”
You lose your livelihood and a lot of independence, and it’s very hard to ask for help because people don’t understand what you’re going through.
“The pain is invisible because I don’t look ill.”
My mum can notice when I’m in pain, but everyday people will say to me ‘you look fine’. I worry that they think it’s all in my head, I became paranoid and suspicious of people, so I do avoid going to places.
I've tried a number of things to help manage my pain. Deep breathing exercises and mindfulness help a lot, as I tense up when I’m in a lot of pain. My acupressure pen has also been helpful for my ankles – it helps stave of the pain so I can still walk.