pGALS Assessment
pGALS (paediatric Gait, Arms, Legs and Spine) is a simple, quick approach to assessing a child with an MSK concern. pGALS is validated in school-aged children but younger children can easily do it also. pGALS takes approximately 1–2 minutes to perform and helps to discern abnormal joints due to a variety of causes (rheumatological, orthopaedic, neurological and neuromuscular). pGALS is not diagnostic of any disease. The findings need to be interpreted in the clinical context but are key to a differential diagnosis and guiding further assessment and investigations.
pGALS is similar to the adult GALS examination with a number of features added. A table of the key differences can be found here.
The sequence of the pGALS examination does not have to be performed in the order of gait, arms, legs and spine; it is presented in that manner to aid learning.
If an abnormality is detected using pGALS, a more detailed examination of the affected joint(s) can be undertaken via a pREMS approach (paediatric Regional Examination of the Musculoskeletal System). This should include examination of the joint above, below and opposite in addition to the area of concern.
Screening questions
Three screening questions are first asked as part of the pGALS:
Question: Do you (or does your child) have any pain or stiffness in your (their) muscles, joints or back?
Rationale: emphasis on common symptoms of a musculoskeletal problem
Question: Do you (or does your child) dress yourself (him/herself) completely without any difficulty? *
Rationale: emphasis on upper limb function
Question: Do you (or your child) walk up and down stairs without any difficulty? *
Rationale: emphasis on lower limb function
*If unable to comment on difficulty dressing or use of stairs then alternative questions include: Can the child squat or reach up without difficulty?
General approach
- Introduce yourself and obtain (verbal) consent/assent.
- Chaperone as necessary.
- Observe child walking into clinic room or playing at rest.
- Appropriately expose (be aware of cultural sensitivity and gender).
- Watch for non-verbal signs of distress/pain (e.g. facial expression, withdrawing limb).
- Carefully check for symmetry and look for joint swelling, abnormal posture, muscle wasting.
- Perform the whole examination – joint involvement may not be obvious from the history and may have been overlooked by the parent or carer. Although changes may be subtle, joint involvement can be helpful to establish the diagnosis.
- A ‘copy me’ approach can be particularly helpful, sitting opposite the child – often makes the examination a form of play and helps with younger children.
- With younger children and those who may not be able to follow this approach, particular emphasis is placed upon observation and being opportunistic/using distraction techniques whilst examining.
- Further advice on general approach.
Individual steps of pGALS - Gait
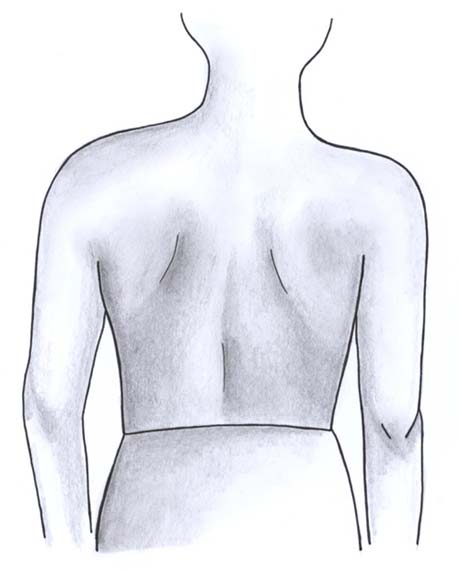
- Whilst child is standing, observe from the front, sides and back. Check for general demeanour, body posture and proportions (trunk/limbs considering short stature/ marfanoid syndromes). Check for any evidence of dysmorphism. Inspect the skin (rashes/bruising/scars/elasticity).
- Observe child walking, turning and returning back. Consider normal patterns of walking and milestones as you observe.
- Ask: “walk on your tiptoes” then “walk on your heels”.
- Check for arm movement as they walk.
- Check for trunk stability/posture as they walk.
- Getting the child to run up and down may help them settle and may demonstrate subtle limp.
Assesses:
- posture, balance, body habitus, skin rashes
- muscle bulk (atrophy), leg alignment (valgus or varus), spine (scoliosis/kyphosis)
- joint swelling, leg length difference
- foot posture (specifically arches when on tiptoes)
- joints of the feet, ankles.
Individual steps of pGALS - Arms
Ask: “Hold your hands straight out in front of you keeping your elbows straight”, specifically looking for nail changes, skin changes (e.g. psoriasis).
Assesses:
- forward flexion of the shoulders, elbow extension
- supination
- wrist extension, finger extension
- May give indication of hypermobility (if not symmetrical, then consider pathology).
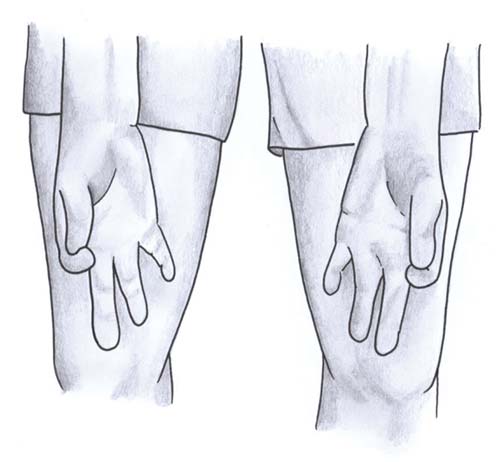
Ask: “Turn your hands over and make a fist”. Look at muscle bulk of thenar and hypothenar eminences.
Assesses:
- elbow and wrist supination
- finger flexion, grip strength.
Ask: “Pinch index finger and thumb together”, followed by “Touch the tips of your other fingers with thumbs”.
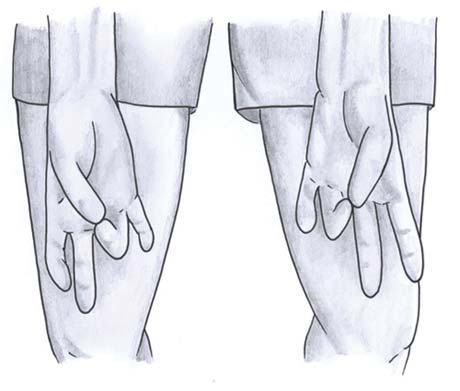
Assesses:
- manual dexterity, fine motor function
- coordination of finger joints.
- May give indication of hypermobility (if not symmetrical, then consider pathology).
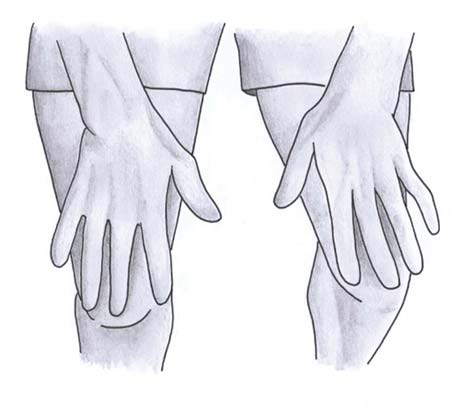
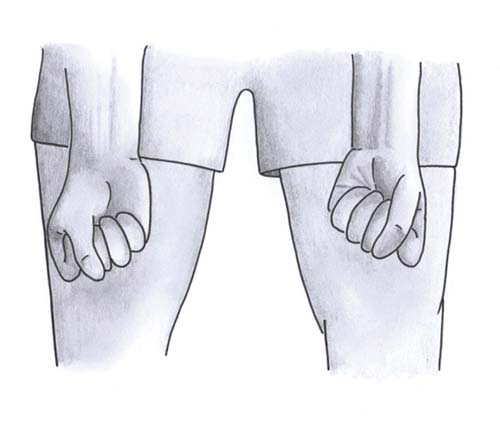
Ask: “Hold your hands straight out and I will carefully press across your knuckle joints”.
Assesses:
- Metacarpophalangeal (MCP) joints for the presence of any pain or swelling.
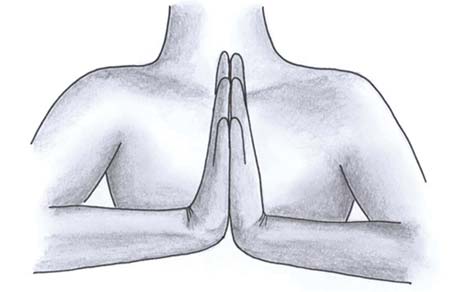
Ask: “Place your hands together – palm to palm” followed by “back to back”.
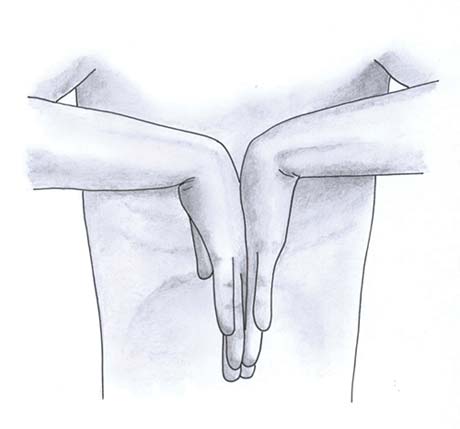
Assesses:
- extension of finger joints
- wrist extension and flexion
- elbow flexion
- coordination of finger joints.
- May give indication of hypermobility (if not symmetrical, then consider pathology).
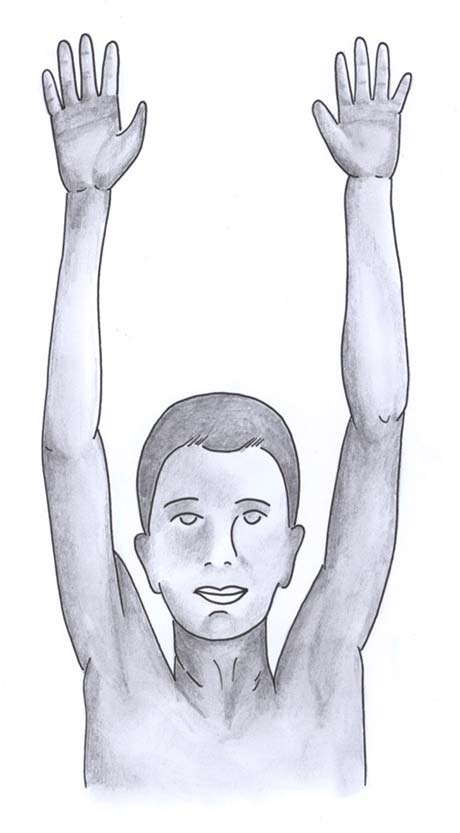
Ask: “Reach up and ‘touch the sky’ then look at the ceiling.”
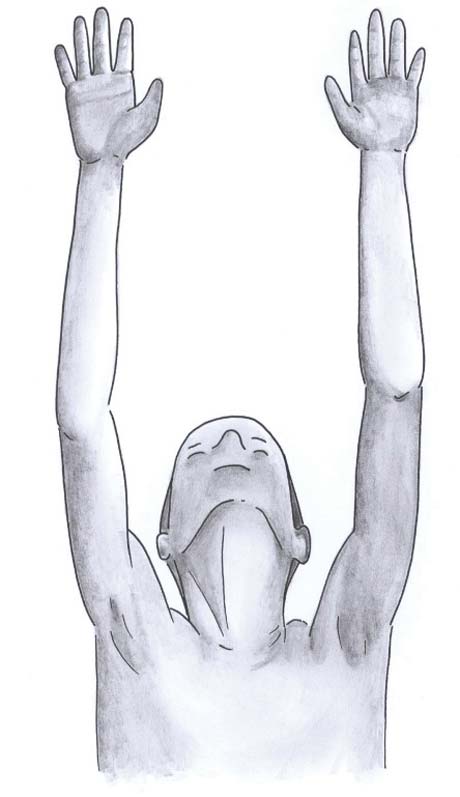
Assesses:
- neck extension
- shoulder abduction
- elbow and wrist extension.
- May give indication of hypermobility (if not symmetrical, then consider pathology).
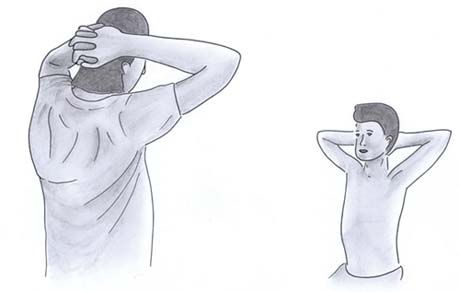
Ask: “Place your hands behind your neck.” Look at elbows for skin changes, skin elasticity.
Assesses:
- shoulder abduction
- external rotation of the shoulders
- elbow flexion.
- May give indication of hypermobility (if not symmetrical, then consider pathology).
Individual steps of pGALS - Legs

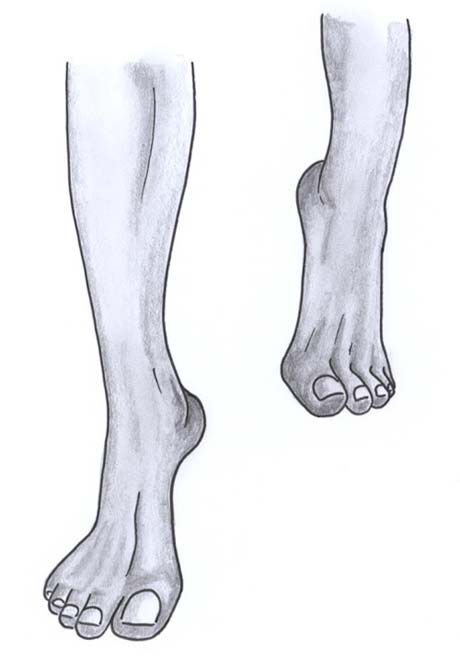
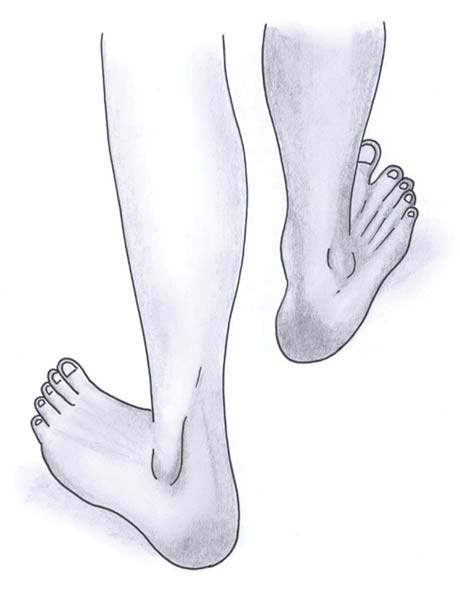
- Observe first – inspect for a leg length discrepancy, soles of the feet, posture, muscle bulk, swelling, scars, alignment.
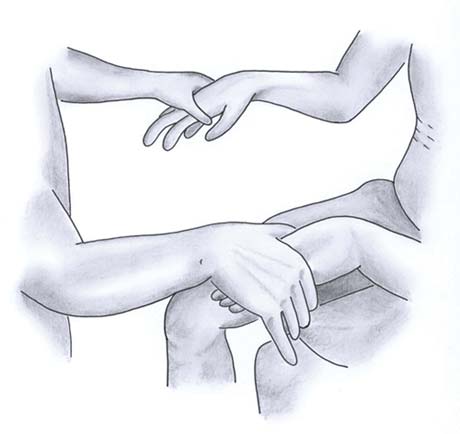
- With the child lying supine, palpate for an effusion of the knee (patellar tap, sweep/bulge test).
Assesses:
- knee effusions, crepitus of the knee
- knee flexion and extension
- hip flexion and internal rotation.

- Ask: “Bend your knee and bring your foot back towards your buttock” – check for symmetry.

- Ensure the legs are stretched out straight to full extension (lack of full knee extension can be an indicator of joint disease) – holding the child’s feet may help to assess full extension/passive hyperextension.
- Excess hyperextension may give indication of hypermobility (if not symmetrical, then consider pathology).
- Passively flex the child's hip followed by assessing internal rotation (with hand placed over the knee, palpating for crepitus).
Individual steps of pGALS - Spine

Ask: “Touch your shoulder with your ear”.
Assesses:
- cervical spine lateral flexion.
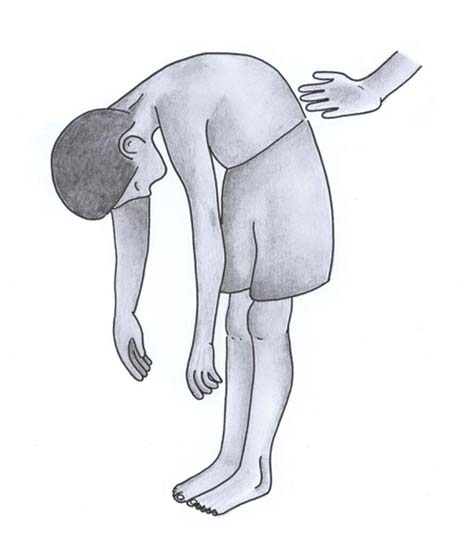
With the child standing, ask: “Bend forward and touch your toes”, specifically inspecting the spine for scoliosis, lordosis, kyphosis.
Assesses:
- forward flexion of the spine (thoraco-lumbar).
- May give indication of hypermobility if can place hands on the floor.
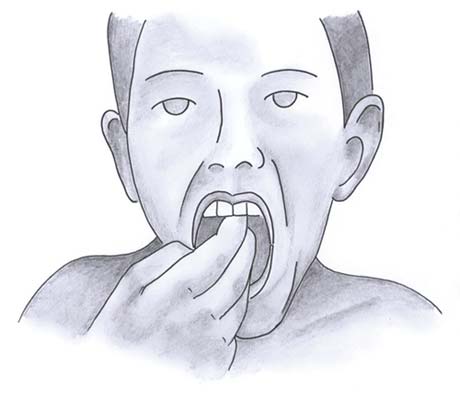
Ask: “Place your own 3 fingers in your mouth.”
Assesses:
- temporomandibular joints (ensure to look for deviation of the jaw or a small jaw micrognathia). Listen for clicks.
Performing virtual pGALS
pGALS can be performed whilst conducting a virtual consultation. Ensure the child and family are aware beforehand of what will happen. Instructions/graphics of the various pGALS manoeuvres can be sent beforehand to allow the family to partake fully. The focus on the consultation is on observation and function. Remember pGALS can be performed in any order to suit the required scenario and technology set-up or timing.
pGALS Assessment: A step by step guide.
Further information on pGALS
- Summary of pGALS assessment and checklist.
- pGALS app contains breakdown of pGALS steps, top tips and further pGALS resources with multiple language translations (all free and available as PDF versions), it can be downloaded from PMM.
- pGALSplus – Toolkit based on pGALS containing questions and assessments to aid with the identification of children with MSK related issues.
- Review of normal gait, normal variants and motor milestones.
- Abnormal gait patterns.
- Top tips and key points of approaching a limping child.
- A publication relating to the use of the pGALS approach.
- pGALS has been translated into over 21 different languages. A downloadable PDF summary of pGALS in a variety of languages can be found on PMM.
- A proforma for recording pGALS can be downloaded as a PDF from PMM.