First of its kind study for children with arthritis reveals possible new disease targets
02 July 2025
Researchers have been able to see what happens in the inflamed joints of children with arthritis, giving insight into why treatments affect children differently.
Groundbreaking new study
A new, groundbreaking study by researchers from University of Birmingham, UCL, Great Ormond Street Hospital and Birmingham Women’s and Children’s Hospital has revealed important clues into what is driving disease in children with arthritis.
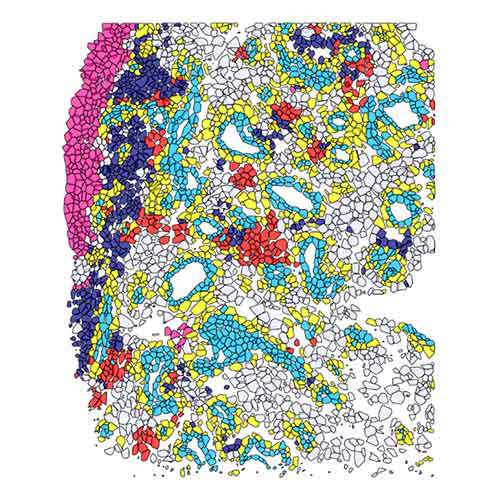
Cutting-edge techniques have allowed scientists for the first time to uncover the unique architecture of cells and signals inside the joint as inflammation takes hold.
The new study published in Science Translational Medicine looks at arthritis in children, caused by the immune system mistakenly attacking joints. Juvenile idiopathic arthritis affects more than 10,000 children in the UK. It causes swelling, stiffness and pain in the joints over years or decades, leading to damage of the joints and long-term disability. Whilst treatments are available to manage the condition, and in some cases achieve remission, there is no cure. It can take time to find which treatment works for each person. Treatments don’t work in the same way for every child, suggesting there are hidden differences between individuals that we are only beginning to understand.
Deepening the scientific and clinical community’s understanding of the condition is vital if more effective treatments are to be found, and undertaking biopsies in young children provides a new way forward. Working with families of children with arthritis opened the door to this study, as the families advocated for the potential of the study, agreeing that the procedure would be acceptable to families, especially compared to living with a chronic inflammatory disease.
In a world first, tiny tissue samples were collected from the joint lining when children were having medicine injected into the joint. These samples were then analysed with advanced imaging and gene-profiling technologies. The fine resolution maps of the joints revealed differences between children of different ages and cell changes in those with more severe disease. These unique cellular fingerprints may help researchers understand why some drugs work better for some children, and not others. The joints of children with arthritis looked significantly different to those with adults, demonstrating the need to understand arthritis in children better.
Professor Adam Croft, Versus Arthritis Professor of Rheumatology at the University of Birmingham and chief investigator of the study said:
“We know how frustrating it can be for families and young people to find a drug that best works for their arthritis. Finding ways to better predict which medicines will be beneficial for a particular child would mean we were able to treat the disease more rapidly and effectively. To achieve this goal, we first needed to understand what cells make-up the lining of the joint where the inflammation occurs. Equipped with that knowledge, we can now start to tackle the next challenge, determining how these cellular fingerprints within the joint tissue can help us predict which drug will work best, ensuring we give the right drug, to the right child, at the right stage of their disease.”
One of the children who took part in the study was Aurelia, from London, who was diagnosed with arthritis after injuring her knee while on holiday.
 “Aurelia is a sporty child and loves art, drama, music and ballet. We noticed pain and swelling of her knee whilst on holiday. We thought perhaps she had injured it playing, but when this didn't get better and she was struggling to walk, we realised something else was wrong. She was referred to the Rheumatology team at Great Ormond Street Hospital who diagnosed her with arthritis. This came as a bit of a shock given how active she is!
“Aurelia is a sporty child and loves art, drama, music and ballet. We noticed pain and swelling of her knee whilst on holiday. We thought perhaps she had injured it playing, but when this didn't get better and she was struggling to walk, we realised something else was wrong. She was referred to the Rheumatology team at Great Ormond Street Hospital who diagnosed her with arthritis. This came as a bit of a shock given how active she is!
“They offered her a steroid injection in her knee under general anaesthetic to alleviate the symptoms. The team asked if we were happy for her to take part in this research study and collect some tissue samples at the same time.
“We were keen for her to be involved, as there’s still a lot of unknowns with arthritis in children, and not all treatments can work. Given that she was already having an anaesthetic, and it wasn’t an additional operation for her, it was a great opportunity for researchers to take samples and to be better able to study the conditions. We hope the study will help other families with children in similar positions to us,” explained Aurelia’s mum, Emily.
Professor Lucy Wedderburn, University College London Great Ormond Street Institute of Child Health and Consultant of Paediatric Rheumatology at Great Ormond Street Hospital said:
“This study represents a real step change in our work with children and young people who live with arthritis, and has been a huge team effort. Rather than having to rely on blood tests which often do not tell us accurately what is happening in the joint, we can now directly analyse the joint lining, across different types of childhood arthritis and different ages. Our findings show that younger children have different types of immune cells invading their joints compared to older children. Samples from children with arthritis looked different to adult samples, with a different make up of immune cells, blood vessels and distinct connective tissue cells. This suggests that treatments may need to vary depending on age and shows why we can’t just extend studies from adult studies to understand arthritis in children.”
The study was funded by the Medical Research Council, Versus Arthritis, National Institute of Health and Care Research, Great Ormond Street Hospital Charity, amongst others, and delivered through the National Institute for Health and Care Research (NIHR) Birmingham Biomedical Research Centre (BRC).
Lucy Donaldson, Director of Research at Versus Arthritis said:
“People with arthritis should never be reduced to just their condition. Each person deserves to be treated holistically as an individual, including, of course, children and young people with arthritis.
“We are very proud to invest in truly innovative research like the MAPJAG study which is helping us to better understand the individual differences between young people with juvenile arthritis.
“The MAPJAG team’s findings clearly show that children and young people aren't just small adults, but have a different "cellular fingerprint". Importantly the team have also shown that this can change with age. The findings can give real hope to all those families that more can be done, sooner, to enable young people with arthritis to live the lives they choose.”
Tissue Research in Childhood Arthritis (TRICIA)
A wider programme of work, made possible by a Medical Research Council partnership award known as Tissue Research in Childhood Arthritis (TRICIA), supports the infrastructure needed for multi-centre tissue research of the joint. In future, it is hoped that a larger study, involving more centres will allow researchers to dig deeper into the remaining questions about how best to tailor treatments for individual patients.
Instrumental to driving this research forward was Dr Eslam Al-Abadi, a study investigator from the Birmingham Women’s and Children’s Hospital NHS Foundation Trust, who sadly passed away before publication. His incredible efforts in seeking to improve the care of children with this disease are gratefully acknowledged.