What is reactive arthritis?
Reactive arthritis causes you to have extremely painful, swollen joints and can make you feel very tired. It can affect your joints after you’ve had an infection somewhere else in your body, such as a tummy bug, diarrhoea (die-a-ree-ah), or a throat infection.
The most common joints to be affected are the knees and ankles.
It’s sometimes called Reiter syndrome and can affect people of any age, including children.
Reactive arthritis is a type of inflammatory arthritis. Unlike other types of inflammatory arthritis, for many people reactive arthritis lasts a relatively short amount of time - usually around three months to a year.
However, some people find it lasts longer and can have random flare-ups years after they first get it.
The pain, swelling and extreme tiredness of reactive arthritis come after the initial infection. The infection itself may have been so mild you barely noticed it.
It is not yet known exactly why infections trigger reactive arthritis. One theory is that once your immune system has dealt with the infection, fragments of bacteria travel through your bloodstream and collect in the lining of your joints. Your immune system then reacts by causing joint inflammation.
Most people diagnosed with reactive arthritis find they have good days and bad days. It usually clears up within six months without leaving any lasting problems. However, a small number of people do go on to develop another type of arthritis that needs long-term treatment.
Causes
The most common causes of reactive arthritis are:
- stomach upsets
- diarrhoea
- other infections in the gut
- a throat infection - usually caused by a streptococcus bacteria (strep-toe-cok-us).
- slapped cheek syndrome
- glandular fever.
The infection that causes reactive arthritis can be so mild that you may not feel unwell, until you’re aware of the pain in your joints.
It can also follow an infection of the genitals or a sexually transmitted infection (STI), such as chlamydia (kluh-mi-dee-uh).
Chlamydia has no obvious symptoms, especially in women, but may cause pain when passing urine or a discharge from the vagina or penis. If you’re worried, speak to your GP or a sexual health clinic.
We don’t yet know why some people get reactive arthritis, but we do know that it’s linked to a gene that some people inherit, called HLA-B27. These people seem to be more likely to develop reactive arthritis and to get it more than once in their life.
Does it run in families?
You can’t pass reactive arthritis on to your children. However, they can inherit the HLA-B27 gene, which could slightly increase their chance of getting the condition. This doesn’t mean that by having this gene they’ll definitely get reactive arthritis. However, the condition tends to be more common in people with HLA-B27.
Around 1 in every 10 people in the UK carry this gene.
Symptoms
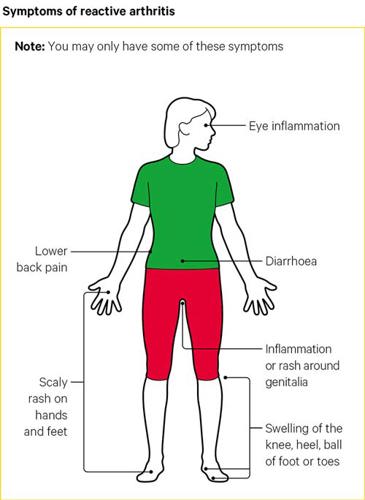
The first signs of reactive arthritis are often:
- painful and swollen joints, usually in the ankles or knees
- sausage-like swelling of fingers or toes
- puffy, sore, red eyes, often with a mucus discharge – known as conjunctivitis
- extreme, unexplained tiredness, known as fatigue
You may notice that your knees, ankles or toes suddenly become swollen, stiff and painful to move. Or the swelling may appear gradually over a few days.
Reactive arthritis can also affect other joints, such as your fingers, wrists, elbows and the joints at the base of your spine, known as the sacroiliac joints (sac-row-il-i-ak). It can also cause inflammation in the tendons around your joints, such as the Achilles tendon (a-kill-eez) which runs down the back of your ankle.
You may find your whole finger or toe swells up if both the tendons and joints become affected at the same time. This is often called sausage digit or dactylitis (dak-til-eye-tis).
Other symptoms
Joint pain and swelling are the main symptoms of reactive arthritis. However, it can cause other problems, such as:
- scaly rashes over your hands or feet
- diarrhoea, which may start some time before the reactive arthritis
- mouth ulcers
- stinging and sometimes discharge when you wee (called urethritis); this is caused by inflammation of the urethra (you-ree-th-ra)
- a sore rash over the end of your penis
- weight loss
- fever.
If you have any of these symptoms, it’s important you contact your GP surgery, so you can be diagnosed quickly.
Diagnosis
There isn’t a specific test for reactive arthritis. Before making a diagnosis, your doctor will consider whether:
- you’ve recently had an infection that could be linked to the sudden pain and swelling in your joints, especially in your knees or ankles
- you have other visible symptoms, such as a rash over the palms of your hands or soles of your feet, or red painful eyes, as well as joint inflammation.
Your doctor will probably take a blood sample, to make sure your problems haven’t been caused by another type of inflammatory arthritis. Blood tests can rule out conditions such as rheumatoid arthritis, psoriatic arthritis (saw-ree-at-ik arth-ri-tis), Behçet’s syndrome (be-chets sin-drome) and gout (gowt).
A blood sample can also:
- show the levels of inflammation in your body
- see if you have the HLA-B27 gene.
Your doctor may also ask for a urine or stool sample, or take swabs from your throat, penis or vagina, to check for signs of inflammation or infection.
If your eyes are red and sore, you may be referred to an eye specialist, called an ophthalmologist (of-thal-mol-uh-jist). They will look into whether you have conjunctivitis or more serious inflammation of the eye, known as iritis or uveitis.
Treatment
There are three ways people with reactive arthritis can be treated:
Treating the infection
If you are still showing signs of infection, your doctor will prescribe antibiotics. This won’t treat the inflammation in the joint, but should get rid of the bacteria that caused the infection in the first place.
If you’ve had a stomach upset, bowel or genital tract infection, you’ll probably be given oral antibiotics. Conjunctivitis is often treated with eye drops or ointment. More severe inflammatory eye conditions, such as iritis (eye-rye-tis) or uveitis (you-vee-eye-tis), may need steroid eye drops.
Antibiotic treatment shouldn’t last longer than four weeks.
Treating the inflammation
If you have mild to moderate pain and inflammation, you doctor may prescribe non-steroidal anti-inflammatory drugs (NSAIDs). These include ibuprofen or naproxen.
Before prescribing NSAIDs, your doctor will consider your medical and lifestyle history for other risks, such as:
- smoking
- circulation problems
- high blood pressure
- high cholesterol
- diabetes.
You’ll usually be given the lowest effective dose of NSAID for as short a time as possible.
If you have a history of stomach problems, your doctor may prescribe a proton pump inhibitor (PPI) with the NSAID. This will stop you getting stomach upsets, indigestion, or damage to the lining of your stomach.
A major part of reactive arthritis is the fatigue – or extreme tiredness – it causes. It’s important to recognise when you’re tired and need to rest, but it’s also important to keep up some level of activity. Bed rest can do more harm than good.
When your symptoms are at their worst, you should try to get plenty of rest and avoid putting too much strain on the affected joint. If you can gently move it, this should stop it becoming too stiff.
After a couple of days, when the pain starts to improve, try to move the sore joint more by doing some light stretching and strengthening exercises. This will help support the muscles and tendons around it.
Your doctor may refer you to an occupational therapist or a physiotherapist (fizz-ee-oh-thair-row-pist).
A physiotherapist can show you exercises to strengthen the muscles that support your joints.
An occupational therapist can help you find ways to stop your pain getting worse and show you how to work or do tasks without putting too much strain on your joints. They can show you equipment, aids or adaptations. Equipment such as hand and wrist supports, or heel and shoe pads can help ease your inflammation and pain.
They can also advise you on ways to reduce the strain on your joints by changing how you:
- sit or stand
- have your workstation
- move.
Ice packs and heat pads can also help with joint pain and swelling. Remember to protect your skin by wrapping a cloth around the pack.
You can either buy an ice pack from a pharmacy or use a bag of frozen vegetables, wrapped in a damp towel. Place the pack on your affected joint for 10 to 20 minutes.
Check the skin colour under the ice pack at least once during that time. The area should be very pink and should never have a blue tinge. The ice pack can be re-applied every two hours.
Heat packs can be useful if your muscles around the joint feel sore and tense. You can use reusable heat pads, a microwaveable wheat bag, or a hot water bottle, wrapped in a dry towel, on the painful area for up to 20 minutes. If the area starts to feel too warm, place an extra towel between the heat pack and your skin.
Treating the arthritis
If your symptoms are really bad and other treatments haven’t helped, your doctor may recommend an injection to remove the fluid that is causing the swelling in your joint. This is called aspiration.
Once the inflammation has gone down, you may be given a steroid injection into the joint. This is often used to help with knee pain.
If your reactive arthritis is bad, you may need a steroid injected into a muscle. This will help the steroid spread through your body. Alternatively, you may be given low-dose steroid tablets, which often work very well in the short term.
If these treatments haven’t helped after a few weeks and your symptoms are still bad, you may be prescribed disease-modifying anti-rheumatic drugs (DMARDs), such as:
and, occasionally:
- methotrexate, or
- azathioprine.
DMARDs work on the underlying condition, rather than treating symptoms. They're not painkillers, but they'll reduce pain, swelling and stiffness over weeks or months by slowing down the condition and its effects on the joints.
There are two kinds you may be prescribed for reactive arthritis: conventional DMARDs and biological therapies.
They can take between six weeks and six months to work. They can be prescribed on their own or with steroids or NSAIDs.
DMARDs can cause changes in your blood or liver, so it's important to have regular blood tests while taking them. Methotrexate and sulfasalazine can sometimes make you feel sick, have diarrhoea, headaches or lose your appetite, at first. These are common side effects and should clear up, once your body gets used to the drug.
Speak to your doctor if your medication isn’t working, or you’re worried about side effects.
If conventional DMARDs don’t work for you, you may be prescribed injections of a biological therapy. These are also called biologics.
Biologics are a newer type of drug that are prescribed when conventional DMARDs haven’t worked. DMARDs and biologic therapies can lower your body’s ability to fight infections, so you should try to avoid people who have bacterial illnesses such as tummy bugs, colds, or a sore throat.
Tell your doctor straight away if you develop any signs of infection, such as:
- a sore throat or fever
- any unexplained bruising or bleeding
- breathlessness
- jaundice (when the eyes and skin turn yellow).
You should also see your doctor if you come into contact with anyone who has chickenpox or shingles, or if you develop chickenpox or shingles yourself.
Tips to reduce your risk of infection
- Try to avoid close contact with people you know have an infection.
- Wash your hands regularly and carry around a small bottle of antibacterial hand gel.
- Keep your mouth clean by brushing your teeth regularly.
- Stop smoking if you’re a smoker.
- Make sure your food is stored and prepared properly.
- Try to keep your house clean and hygienic, especially the kitchen, bathrooms and toilets.
If you are prescribed a drug you may find more information about it here.
Living with reactive arthritis
As well as prescribed treatments, there are a number of things you can do yourself.
Rest and exercise
When your joints are inflamed and painful, you can feel tired and generally unwell. Fatigue plays a major role in reactive arthritis and can have a huge impact on all aspects of your life. It’s important that you and people around you recognise this.
It’s equally as important to keep moving. You could try:
- swimming in a heated pool - this allows you to exercise while the water supports your weight
- stretching exercises - keep the muscles and tendons that support the joint strong and supple
- talking to your line manager about working shorter hours
- asking whether you can avoid any activities that are too demanding
- making your workstation better suited to your condition.
Your doctor can refer you to a physiotherapist or occupational therapist for specific advice.
Getting a good night’s sleep and recognising when you need to relax are really important to your recovery. If you’re finding it difficult to wind down relaxation techniques, such as breathing exercises, mindfulness or meditation, may help.
A good bedtime routine can also make you feel better. Try to get an early night and give yourself an hour before to have a warm bath and relax, try to avoid using your computer, phone or TV in that hour, as they can disrupt your sleep.
Diet
There is no specific diet proven to help reactive arthritis, but a well-balanced diet is important to your general health and wellbeing.
Some people say rose hip extract and fish body oil reduce their need for anti-inflammatory drugs. They are known to support your immune system and help reduce inflammation and joint damage.
Complementary and alternative treatments
Complementary and alternative treatments, such as acupuncture (ak-you-punk-cher), massage and supplements, may help your symptoms.
There can be risks associated with some complementary and alternative treatments. You should let your doctor know about any complementary therapies you’re considering, as some can react with prescribed medications.
Before you make an appointment, check that your therapist is registered with an official governing body or has a set code of ethics and is insured.
Research and new developments
Versus Arthritis continues to support research into reactive arthritis. We now understand more about how infections can over-stimulating the immune system and trigger reactive arthritis.
Continued research into arthritis could lead us to develop more effective treatments in the future.
We’re also researching ways to treat the pain arthritis causes and looking into ways to reduce its impact on daily life.