Understanding childhood pain is vital to improve future treatments
14 October 2020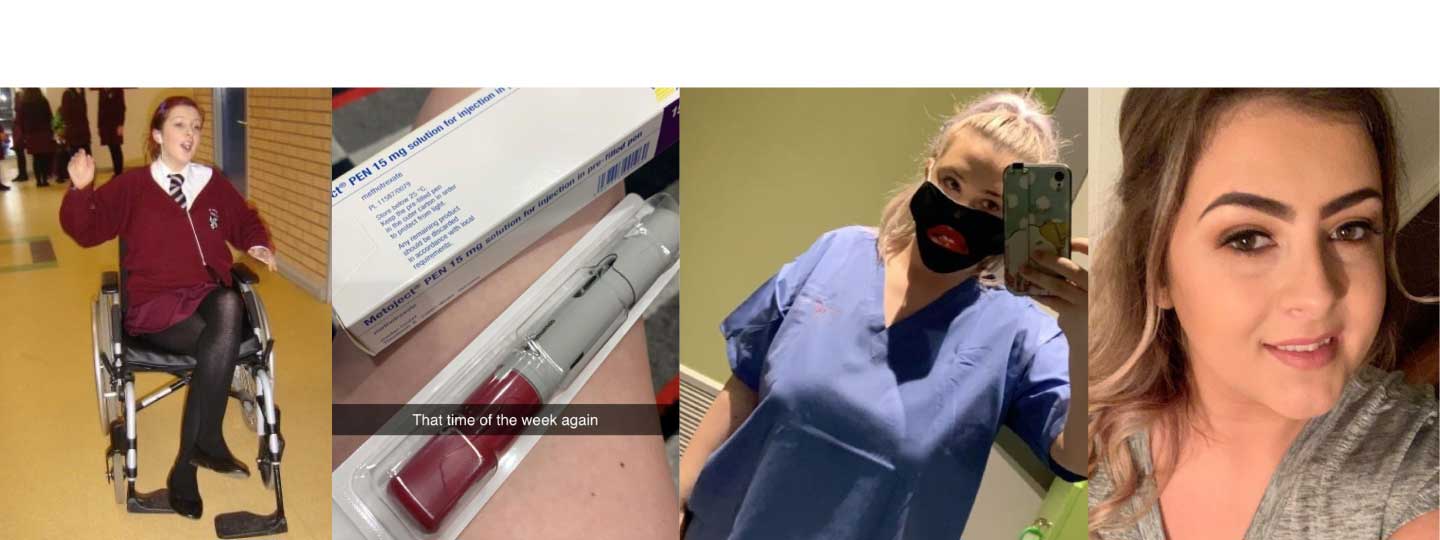
The Lancet Child and Adolescent Health Commission’s report is the first ever to address paediatric pain and recommend what more can be done to help children and young people.
This work has been co-funded by Versus Arthritis and the Mayday Fund and led by the University of Bath‘s Centre for Pain Research.
Why is change needed?
Childhood pain is still very poorly understood. The last major intervention in treating childhood pain came in the 1980s when, remarkably, for the first time, it was recognised that babies experienced pain.
Astonishingly, up until that point, a number of routine and major operations, including for heart surgery, were carried out without anaesthetics.
The report speculates that much of what we do (or fail to do) for children in pain today, might come to be seen as unacceptable or unethical in the next 40 years.
The report calls for four key areas of improvement:
- To make childhood pain matter
- to make it understood
- to make it visible and
- to make it better
Achieving these goals would transform the lives of children for the better.
Pain is complicated
Understanding pain in children is complicated and there’s still more research to be done to learn more about how babies, children and young people experience and respond to pain and treatments.
As we know, one-size treatments don’t work for everyone, particularly when prescribing drugs and painkillers. A holistic perspective needs to be taken to look collectively at the person, their condition, and any other medical factors.
This applies to childhood pain just as much as adults. As we’ve learnt more about children’s physiology and treatments, it has become clear that they are very different and can’t simply be treated in the same way as adults.
Caitriona’s story
When 12-year-old Caitriona went to her doctor because she was experiencing pain and swelling in her ankle, no one knew quite what was up.
Initially written-off as ‘just a sprain’ which would go away, she would spend the next six months living in almost constant pain until interventions from a diligent doctor referred her to a specialist.
Caitriona was diagnosed with juvenile idiopathic arthritis, a condition the now 28-year-old has lived with and managed ever since.
Caitriona now works in law, alongside volunteering for Versus Arthritis helping other young people going through similar diagnoses.
“I think this issue has been swept under the carpet for too long. Still today, over 15 years on from my diagnosis with arthritis, I find people, including medical professionals, unaware of the condition or its effects on my day-to-day life.
“And when I speak to other young people, I find that sadly, very little seems to have changed in terms of how they experience pain or the support they receive.
“Versus Arthritis were so pivotal in supporting me when I was first diagnosed that it’s fantastic to be able to give back and help other young people. Working together and talking as a community we’re able to share our experiences and shape interventions like this.”
How can we make a difference?
Dr Emma Fisher, Versus Arthritis Career Development Fellow at the University of Bath, who led the work explains:
“This really matters, both for those experiencing pain and those around them but also across wider society. We know that chronic pain experienced in childhood is likely to feed through to adulthood and this has long-term health and economic costs associated. “
“This Lancet Child and Adolescent Health Commission is a call to action on funders, researchers and policymakers more broadly to sit up and listen to the fact that too many of our young people are in pain and need help.”
Zoe Chivers, Head of Services at Versus Arthritis says:
"People living with arthritis deal with the dismissal of their condition every day and the Commission findings detail the consequences of this for children in pain.
"Parents tell us about the struggle they have convincing their GP that their child's illness is more than growing pains; we know that the existence of specialist child rheumatology services can make the difference between walking to school or needing a wheelchair.
"As a society we need to understand that dismissal of arthritis comes at high price and that adults and children living in pain with the condition should no longer be expected to pay it.”
Get the support you need
- If you would like to talk to someone, you can call our free helpline on 0800 5200 520 (Monday to Friday, 9am to 8pm)
- Talk to our arthritis virtual assistant, 24/7
- Join our online community
- Stay in touch and follow us on Twitter, Facebook and Instagram.