Malcolm’s story: “Gout is treatable, so get informed and be involved in your own care”
13 July 2023
Malcolm, 65, didn’t know much about gout when he was diagnosed. Like many people, he only had heard unhelpful myths and stereotypes.
“I imagined an old gent in the Victorian times, who drank too much port and had his foot wrapped up in bandages,” Malcolm says. “But I was quite physically active, had a good diet and I didn’t really drink.”
People used to think that gout was caused by overeating and drinking too much alcohol. And while this can make gout attacks more likely, it’s not the whole story.
The truth is gout is a very painful condition, which should be taken more seriously. Plus, it can be caused by lots of different factors, including your genes.
“The pain was excruciating. It takes over your life. But I want people to know that gout is treatable, just like other conditions like diabetes.”
Here Malcolm shares his experiences living with gout, the treatment he received, and why it’s important to be informed and involved in your own care.
What is gout?
Gout is caused by having too much uric acid (also known as ‘urate’) in your blood.
We all naturally have urate in our blood. It’s completely normal. But if you have too much it can start to cause problems.
“Your body can’t get rid of the uric acid, so it’s got to go somewhere,” explains Malcolm. “So, it starts to turn into lots of sharp, little crystals that build up around your joints and rub together. That’s why it’s so painful. So, to fix it, you’ve got to control your uric acid level. It’s that simple.”
What are the symptoms of gout?
Gout attacks
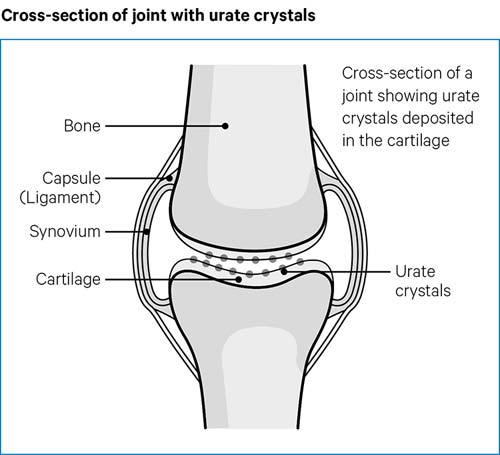
One of the most common symptoms of gout is a ‘gout attack’ or flare-up. This is when urate crystals build up in your joints and spill out into the space between two bones in a joint.
As they rub against the soft lining of your joint (called the synovium), it can make the joint feel painful, tender, red, hot and swollen.
The most common place to experience gout attacks is at the base of the big toe, although other joints can be affected – and this was the case for Malcolm.
“I started to get pain in the joints in my lower limbs, like my big toe,” he says. “It got to the point where I couldn’t wear a shoe. In bed, I couldn’t even stand the weight of a single sheet on my foot.”
“I went to the GP, he took one look at the toe, and said, ‘That’s gout’.”
Tophi
It you have gout, you might also discover small, firm lumps on your skin called tophi. This is when urate crystals collect outside of the joints and can be seen under the skin.
What causes gout?
Sometimes the genes you inherit make it more likely that your kidneys can’t flush the urate out as well as they should. “My father had gout, so I feel it was hereditary,” says Malcolm, noting that his sister also has the condition.
There are also many other factors that can increase your risk of developing gout. For example:
- Gout is four times more common in men than women.
- Although it can affect you at any age, the risk of developing gout is greater the older you get.
- Gout can be caused by chronic kidney disease.
- It can also be caused if you’ve taken a medication that affects how well your kidneys can remove urate from your body for a long period of time.
Treatment for gout
If you’re in the middle of a gout attack, you might take medicines such as:
However, two of the most common medicines to treat and prevent gout attacks are allopurinol and febuxostat. These are called urate lowering therapies (ULTs) because they:
- lower your urate levels
- prevent new crystals from forming
- dissolve away the crystals in your joints

There’s no fixed dose of ULTs, and different people need different doses to get to the right urate level. This level, where the urate crystals dissolve, is sometimes called the saturation point.
“If you're above the saturation point, your body is going be creating urate crystals. If you're below it, you're not going to be creating crystals. It’s that simple,” explains Malcolm.
Initially, Malcolm wasn’t prescribed a high enough dose of allopurinol. “They started me off on the lowest dose of 100mg, which was a drop in the ocean compared to where I needed to be,” he says.
“I spent 18 years in the Royal Marines until I was injured and medically retired. I could switch off the pain then. But I couldn’t manage the pain of gout. I was in a very dark place mentally.”
After taking part in a research study funded by Versus Arthritis, Malcolm learned more about his condition and his uric acid levels. Slowly but surely, the healthcare team increased his dose of allopurinol, and the crystals began to dissolve.
“I’m still on the same dose of allopurinol and I've not had a gout attack since. Your GP should test you every year to see what your uric acid level is. If it’s still above saturation point, then they should consider increasing your dose.”
Like all medicines, ULTs have side effects. Plus, it’s important to remember that they won’t stop attacks of gout straight away. In fact, you might have more attacks within the first six months of stopping them.
ULTs are usually life-long treatments and require yearly check-ups to monitor your urate levels. if your symptoms aren’t getting under control, chat to your doctor about your urate level. Because you might need to be on a higher dose.
Educating yourself
If Malcolm could get give one piece of advice to anyone diagnosed with gout, he’d recommend being “actively involved in your medical care.”
“Get educated about your condition,” he says. “Get relevant information from professional bodies and charities, not just hearsay.
Check out the NHS, EULAR (The European Alliance of Associations for Rheumatology) and Versus Arthritis. Understand what treatment is out there and have those conversations with your GP.
Gout is very treatable. You don’t have to suffer.”
We’re here to help
If you need advice or support, you can:
- Call our free helpline on 0800 5200 520
- Chat to our Arthritis Virtual Assistant
- Join our online community
- Stay in touch and follow us on Twitter, Facebook and Instagram.