What is palindromic rheumatism?
Palindromic rheumatism (pal-in-drom-ic roo-ma-tiz-em) is a form of inflammatory arthritis. It causes attacks or flare-ups of joint pain and inflammation that come and go. The joints look and feel normal between attacks, and the attacks don’t cause any lasting damage to the joints.
It’s sometimes known as palindromic arthritis.
Symptoms
People with palindromic rheumatism usually have no symptoms between attacks. This is different from other types of inflammatory arthritis, such as rheumatoid arthritis, as people with these conditions will have joint problems most of the time.
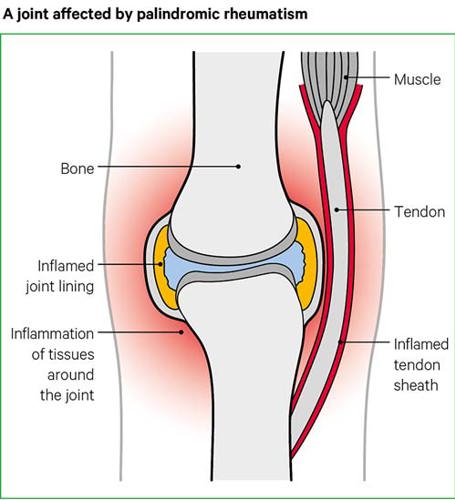
During an attack of palindromic rheumatism, the joints involved – and the tendons and area around them – will feel painful and stiff, and may look swollen. They might also feel tender and hot, and the skin over your joints may look red.
What are attacks of palindromic rheumatism like?
Attacks usually start in one or two joints, often the hands, which quickly become painful, stiff and swollen. Other areas around the affected joints, such as the tendons, may also become painful and swollen. Attacks are sometimes called flares or flare-ups.
Attacks can move from joint to joint, and usually last for a few days. Eventually the attack stops, and your joints and tendons will return to normal.
No matter how often you have them, these attacks are not thought to cause damage to your joints. People with palindromic rheumatism normally feel well between attacks.
Some people feel very tired after having an attack. This is known as fatigue. This fatigue can last for a few days or weeks and might affect you physically. It can also affect your concentration and motivation.
Attacks of palindromic rheumatism come and go. But the pattern of attacks – how often they happen, how long they last and what joints they involve – is different for everyone.
Some people have less than one attack a year, while others have them more than once a week. Some people have attacks that last just a few hours, while some people’s last for several days. You might notice that your attacks are similar each time.
Palindromic rheumatism doesn’t usually affect parts of the body outside the joints and tendons.
However, some people might also have a fever during an attack or develop nodules under the skin, near the affected joints.
Causes
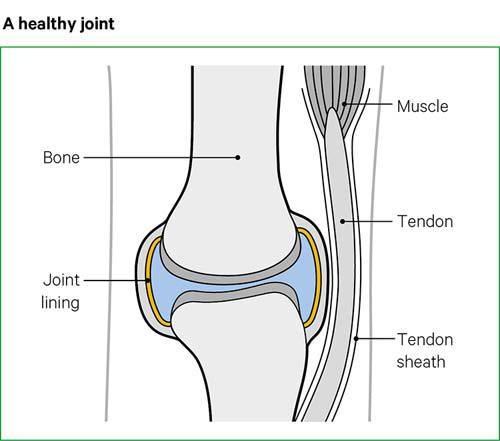
Inflammation is caused by your body’s immune system and is a normal response to injury or infection. In palindromic rheumatism, the immune system attacks your joints by mistake.
Inflammation causes redness, swelling and extra fluid in and around the joints of people with palindromic rheumatism. This is similar to what happens if you have a cut or wound.
We don’t yet know what causes the inflammation in palindromic rheumatism. Although there may be genetic links, other triggers are likely to play a part, such as infection, hormones or injury.
Palindromic rheumatism affects women and men equally. The condition can start at any age, but it rarely affects children.
Diagnosis
Palindromic rheumatism is rare, so your GP may not have seen many cases. It can sometimes be confused with conditions like gout and rheumatoid arthritis.
To confirm the diagnosis and to ensure that treatment is started as soon as possible, your GP should refer you to a rheumatologist (roo-ma-tolo-jist), who is a consultant with specialist knowledge of these types of conditions.
Visiting a doctor
Palindromic rheumatism can’t be diagnosed through one specific test, so a diagnosis will be based on your symptoms, as well as blood tests and scans. Your doctor will ask questions and look at your joints to help rule out other forms of inflammatory arthritis.
Ideally, a doctor should examine you during an attack, before your symptoms disappear. If you can’t get to a doctor during an attack, taking a good-quality photo of the affected joints and keeping a diary of your symptoms can help your doctor make a diagnosis.
Blood tests
Blood tests for erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can be used for a diagnosis, as these show levels of inflammation in your body. Other blood tests can check for antibodies – such as rheumatoid factor, anti-CCP antibodies anti-nuclear antibodies – which can help to diagnose palindromic rheumatism.
X-rays
Palindromic rheumatism doesn’t usually cause any damage your joints. But a doctor may still ask you to have x-rays of your affected joints, so they can rule out other conditions.
How will palindromic rheumatism affect me?
Palindromic rheumatism varies from person to person. Some people find that their symptoms completely disappear between attacks, while others only have attacks occasionally.
However, some people experience more problems over time, and may develop rheumatoid arthritis. This is particularly likely in people whose blood tests show rheumatoid factor or anti-CCP, which can be positive in rheumatoid arthritis.
While palindromic rheumatism doesn’t cause any permanent damage to the joints, rheumatoid arthritis can. Even if you have a positive test result for these antibodies, you won’t necessarily develop rheumatoid arthritis.
Very rarely, a small number of people develop lupus, and this is more likely in people whose blood tests show anti-nuclear antibodies.
Treatments
Once the diagnosis of palindromic rheumatism has been confirmed, your care is likely to be shared between your GP and a rheumatologist.
You might also see a specialist nurse in your rheumatology department. They will all monitor you to make sure you’re not developing another condition that would need different treatment.
Drugs
The main treatments for palindromic rheumatism are drugs to treat the pain, drugs to reduce inflammation, and drugs to treat the condition itself. People respond to treatments in different ways, so it’s important to work with your doctors to find the best treatment for you.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs block inflammation and are used to reduce pain, stiffness and inflammation during attacks.
Your symptoms may improve when you take these drugs, but the effects aren’t long-lasting, so you might have to take them regularly. If they do work, you’ll need to take them as soon as an attack starts and carry on until after it’s finished.
There are many NSAIDs available, so your doctor will advise you on the best choices for you. Examples of NSAIDs include naproxen and ibuprofen.
NSAIDs can sometimes have side effects, but your doctor will try to reduce the risk of these. This could be giving you the lowest dose that works for you for the shortest possible time, or by prescribing a type of drug called a proton pump inhibitor, which can help reduce the risk of stomach problems.
Steroid injections
Your doctor might suggest a steroid injection if your joints are very painful, or if your ligaments and tendons are inflamed. Steroid injections can be given directly into a joint or a muscle.
These injections aren’t given regularly. They work very quickly, usually within a few days. Some GPs can give them, but they’ll usually be given by your consultant or nurse at the hospital.
Disease-modifying anti-rheumatic drugs (DMARDs)
Disease-modifying anti-rheumatic drugs help by tackling the causes of joint inflammation. They’re used in palindromic rheumatism to reduce symptoms and flare-ups.
Unlike the other drugs mentioned here, DMARDs treat the condition itself rather than just reducing the pain and stiffness it causes.
DMARDs can be used to prevent attacks or reduce the frequency of them in people who have a more severe form of the condition. They can sometimes take a while to start working, so your doctor will advise you to keep taking them regularly.
The most common DMARD used to prevent attacks of palindromic rheumatism is hydroxychloroquine. However, some people may need stronger DMARDs like sulfasalazine or methotrexate.
When taking some DMARDs, you’ll sometimes need to have regular blood monitoring to check for possible side effects, including problems with your liver, kidneys or blood count.
Managing symptoms
There are things you can do which may help ease your symptoms and help with your daily activities.
During an attack
When your pain is very bad, you should rest your joints. You might find wrist splints and insoles for your shoes helpful.
Once the inflammation has settled down, you should start to get moving again by doing gentle exercise. You can also speak to your doctor or rheumatology nurse specialist to see if you should increase your medication.
Ice or heat pads, such as a bag of frozen peas or a hot water bottle, can help ease pain and swelling, although you should take care not to put them directly on your skin. Relaxation exercises can also help.
Pacing your activities will help save your energy and reduce fatigue. A doctor or physiotherapist will be able to give you advice on this.
Exercise
Exercise is important to keep your joints working properly, but you may feel too tired during attacks. You’ll need to find the right balance between exercise and rest.
Your doctor or a physiotherapist will be able to give you advice on suitable forms of exercise such as stretching exercises, and hydrotherapy exercises, which are done in warm water.
Diet and nutrition
No specific diets have been found to affect palindromic rheumatism, but being overweight will put extra strain on your joints, so it’s important to keep to a healthy weight. Eating a healthy, balanced diet with plenty of fresh fruit and vegetables is recommended for your general health.
Some people with palindromic rheumatism believe that a particular food appears to trigger their attacks. If you think this may be the case for you, you can try using a food diary, or a diet in which you stop eating that food, known as an elimination diet.
If you decide to try an elimination diet, you should speak to a registered dietitian. They can make sure you’re cutting out certain foods completely, that you’re not missing out on any important nutrients, and give you any support you need.
Complementary treatments
There’s not very much research that shows the effects of complementary treatments on palindromic rheumatism.
Some people find that fish oils reduce their need for NSAIDs because they have a mild effect on reducing inflammation in the body. Pure fish body oil is thought to be more effective than fish liver oil.
If you want to try complementary medicines or therapies, discuss this with your doctor or nurse specialist first, in case any of the treatments could interact with the medications they’ve given you.
It’s important to go to a therapist who is registered, or one who has a set ethical code and is fully insured.
Related information
Living with palindromic rheumatism
Work
Some people with palindromic rheumatism won’t have many problems with work, but those who have attacks more often or who have severe attacks may have more difficulties.
You may be able to adapt your work – for example, by working shorter hours or moving to a less physically demanding role. You have rights which make sure you’re treated fairly at work, and your employer has a legal obligation to make reasonable adjustments for you at work.
If this isn’t possible, you may need a work assessment and retraining, which can be arranged through your local JobCentre Plus. If you’re unable to work or have mobility problems, benefits are available. A health or social worker, or your local Citizens Advice Bureau will be able to advise you on benefits you can claim.
Access to Work is a scheme in Scotland, England and Wales that gives extra help to people with disabilities or physical and mental health conditions. There is a separate scheme available in Northern Ireland.
Access to Work provides funded or partly-funded grants to help people start work, stay in work, or move into self-employment, and can be used to pay for equipment, support workers, or transport, among other things.
Sex and pregnancy
You might not feel like having sex during attacks because of fatigue and pain, but in between attacks you should be able to have a normal sex life.
There’s nothing to suggest that palindromic rheumatism itself affects your chances of having a family. However, medication, especially DMARDs such as methotrexate, can cause problems during pregnancy or while breastfeeding.
NSAIDs aren’t generally recommended during pregnancy, and some recent research suggests that they can make it more difficult to conceive. The risk of miscarriage may also increase if you take them during the early stages of pregnancy.
If you’re thinking about starting a family, you should discuss your drug treatment with your doctor well in advance so that your medications or dosage can be changed if necessary. You shouldn’t stop taking any of your prescribed drugs without talking to your doctor first.
Research and new developments
We have recently funded research into palindromic rheumatism, which has given new insights into what goes on in the body during an attack or flare and the experiences of people with the condition.
This research used the latest ultrasound and MRI techniques to show that the structures around the outside of the joints are major targets in flares of palindromic rheumatism, and can be affected more than the joint itself. This pattern of inflammation isn’t usually seen in rheumatoid arthritis and might allow doctors to better identify people with palindromic rheumatism.
It’s hoped that a better understanding of the condition will improve ways of managing it and help in developing new treatments.
Zoe’s story

Zoe Lee was diagnosed with palindromic rheumatism five years ago, but the road to getting a diagnosis wasn’t easy.
“It started off as excruciating pain and swelling in my ankles and wrists, but every time I'd manage to get a doctor’s appointment, it would be gone. I think it was one of those things where it was a bit of a grey area for them.
“I'd done some research about arthritis myself, and they just kept telling me I was too young. It just went on and on and on, until one morning I had such a swollen hand that it looked like I had been bitten by a spider.
“The GP just took one look at me and said 'you need to go and have some bloods done, I think we're going to have to refer you to rheumatology'.
“When I went back after being on naproxen and hydroxychloroquine for four weeks, I felt the best I'd ever felt, and I thought perhaps he was going to discharge me. But he sat me down and said I had palindromic rheumatism.
“I remember the things that they were saying to me about the blood tests, and the x-rays, and the risk of A, B, C, and D. I couldn't take it all in. I was convinced that it was just going to go away and that I didn't have to live with it.
“I ended up being started on methotrexate, and I came off that to have my little boy. Since having him it's all got worse. When you're pregnant everything clicks back into place, and you almost don't know that you've got arthritis. then it came back with a vengeance after I had him, which they did warn me would probably happen.
“If I'm having a flare, the best thing for me is to try and keep moving and the pain tends to decrease a lot quicker. This can sometimes be difficult, as my flares often occur during the early hours, but you do what you can to cope.
“I do have tears some days, but my little boy can't fend for himself. He thinks it's great when I have to shuffle down the stairs on my bum!
“When someone says to me 'where have you got arthritis?' I say 'I’ve got a strange kind of it that just jumps from joint to joint'. One week it could be my wrist, the next week it could be my knees, I could have two weeks of being absolutely fine, of not even thinking about it, and then it could be my hips.
“I wish I'd gone to the GP with the research I had done and maybe helped them realise that I am old enough, that there isn't an age limit for arthritis and that it can happen to anybody at any age.
“I tried my hardest to not let it affect my life. But I'm finding now that I'm a mum, running a house, working and trying to live a normal life, it does sometimes get in the way. But believe it or not, the good days really do outweigh the bad.”