What is lupus?
Lupus is a long-term condition that can cause inflammation in the skin, organs, and in various other places in the body.
It’s an autoimmune condition. The immune system, which normally protects us against infection and illness, starts to attack the body’s own tissues instead.
There are two main types of lupus:
- discoid lupus
- systemic lupus erythematosus (SLE).
Discoid lupus only affects the skin, causing rashes. People can get it in one small area on the skin, or it can be widespread.
SLE can affect many parts of the body in several ways. It can range from mild to severe. There is no cure, but early treatment can help to keep symptoms under control.
The rest of this information is about SLE, which we will call lupus.
Symptoms
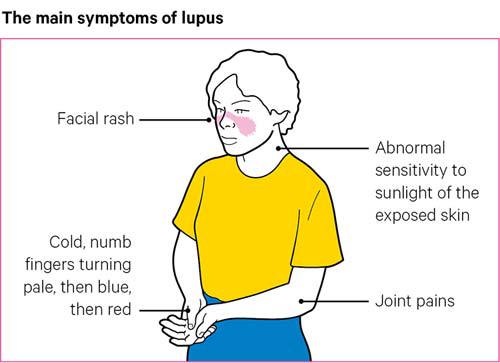
The three most common symptoms of lupus are:
- joint pains
- skin rashes, which may become noticeable after being out in the sun
- extreme tiredness, known as fatigue.
Some people with lupus will only have these symptoms, though they can still have a big impact on daily life.
Other general symptoms are:
- ulcers in the mouth or nose
- hair loss
- fever
- weight loss
- swelling of the lymph glands, in the neck, armpits or groin, or under the chin
- depression
- anxiety.
Lupus can affect many different parts of the body, and when internal organs such as the heart, lungs, brain or kidneys are involved it can be much more serious. It’s important to have regular check-ups, and to report any new symptoms to your healthcare professionals.
Most people will only have one or a few of the possible symptoms, and many people find that the symptoms come and go.
Skin and mouth
It’s common for a rash to develop over parts of the body that are exposed to the sun, most commonly the face, wrists and hands. A butterfly-shaped rash over the cheeks and the bridge of the nose is common in lupus.
Some people notice that their fingers change colour in cold weather, going first very pale, then blue and finally red. This is called Raynaud’s phenomenon and is caused by narrowing of the blood vessels, which reduces the blood supply to the fingers or toes. It can happen in the cold or in stressful situations.
You may develop mouth ulcers. More rarely, ulcers can occur in the nose.
Hair
General thinning of the hair is fairly common among people who have lupus. In some cases, there may be patches where the hair doesn’t grow, and this is called alopecia. Rarely alopecia can be more severe and affect large areas of the scalp. This can be distressing, but once a flare-up is brought under control the hair will usually grow back.
Joints
Joint pain is common in lupus, especially in the small joints of the hands and feet. The pain often moves from joint to joint.
Joint pain, swelling and stiffness can be the main symptoms for some people with lupus. In most cases, lupus is unlikely to cause permanent damage or change the shape of joints. But it can sometimes cause serious joint problems. It’s important you tell your doctor or specialist nurse if you have any new joint pain.
A small number of people with lupus have joint hypermobility. This is when joints are very flexible. It can lead to problems such as joint pain, poor balance and in rare cases dislocation – when a joint pops out of place.
Pain from muscles and joints may be due to a condition called fibromyalgia. This is a widespread pain syndrome and is thought to be caused by an imbalance in the central nervous system that controls and processes pain signals. It’s more common among people with lupus.
If you have pain in your groin, you should see your doctor. This could be a sign of a more serious complication called avascular necrosis. This is when there is a loss of blood supply to bone, which can cause bone damage. Steroid treatment can make this more likely.
Kidneys
People with lupus can have problems with their kidneys. Kidneys play several important roles, including helping to remove toxins from the blood. Until kidney damage is severe, it has no visible symptoms. It often causes high blood pressure.
In most cases if spotted early, kidney problems caused by lupus can be treated successfully. Medication can prevent permanent kidney damage.
Kidney function tests will be a part of your regular check-ups if you have lupus.
Blood and blood vessels
Lupus may also cause anaemia, which is when you have a lack of red blood cells. These cells carry oxygen around the body, and if you don’t have enough of them you can get out of breath and tire quickly. If you have these symptoms you should tell your doctor or nurse specialist.
People with lupus might also have a low number of platelets, cells that help the blood to clot. If you find that you are bruising easily or notice bleeding from the gums or nose you should let your doctor or nurse specialist know. Lupus can also affect your white blood cells, which are important in fighting infections.
Some people with lupus are more at risk of developing blood clots in veins or arteries. This problem is usually caused by antiphospholipid antibodies. These autoantibodies can also affect pregnancy, causing an increased risk of miscarriage.
If blood clots occur blood thinning medication will be needed.
Brain and nervous system
People with lupus may experience anxiety or depression. Some people have dizziness, memory loss or confusion. Lupus can cause fits similar to epilepsy, or very rarely, feelings of paranoia.
Heart and lungs
Lupus can cause high blood pressure, particularly if the kidneys are involved. Steroid tablets, which are often used to treat lupus, can raise blood pressure when used in high doses.
Lupus can also make you more likely to have high cholesterol. Having high levels of cholesterol and high blood pressure can increase the risk of heart attack or strokes.
You should have your blood pressure and cholesterol checked regularly and treated if necessary. Having a healthy diet, a healthy lifestyle, exercising regularly and avoiding foods high in saturated fat and salt, can reduce your cholesterol and your chances of having a heart attack or stroke.
Occasionally lupus directly affects the heart and lungs. More often, it causes inflammation in the lining tissues around the heart, known as pericarditis. It can also cause inflammation in the lining of the lungs, known as pleurisy. Both these conditions cause breathlessness and sharp pains in the chest.
Rarely, large amounts of fluid develop in these lining layers, causing severe breathlessness.
Lupus may also cause narrowing of the blood vessels. This can lead to an increased risk of angina, when a reduced amount of blood gets to the heart muscle.
Other organs
People with lupus can experience swelling of the lymph glands, which may cause discomfort. If you notice this happening, and especially if you also have high temperatures and are losing weight, talk to your doctor or nurse specialist.
Less frequently, lupus can affect the lining tissue of the gut, the gut itself, pancreas, liver or spleen, all of which can cause pain in the stomach.
Very rarely, lupus can cause a painful red eye or changes in your eyesight. If you have any symptoms affecting your eyes, it’s important to see a doctor as soon as possible. If left untreated, eye problems caused by lupus can lead to permanent damage to your eyesight. These issues are very treatable.
Sometimes people with lupus can have an underactive thyroid. This is when the thyroid glands in the neck don’t produce enough hormones. This can lead to problems such as tiredness, weight gain and depression.
A condition known as Sjögren’s syndrome, which causes severe dryness of the eyes and mouth, is more common among people with lupus.
Less commonly, people with lupus can have the inflammatory type of arthritis called rheumatoid arthritis, or a condition known as myositis, which is inflammation of the muscles.
Who gets lupus?
Lupus is much more common among women than men. It’s more common among women of Chinese origin and most common in women of African or Caribbean origin. It tends to be more severe in those of Afro-Caribbean origin. Rarely, lupus can affect children, but it’s unusual before the age of five.
Causes
It’s unclear why some people get lupus. It’s thought to be the result of a mix of genetic, hormonal and environmental factors. For example, the immune system makes proteins called antibodies that fight infection. In lupus, the body also makes autoantibodies that are similar, but attack the body’s own tissues instead. We’re not sure why this happens. There are some factors that probably make this more likely:
- an illness or infection
- strong sunlight
- hormonal changes, such as during puberty
- smoking cigarettes
- some medications – this is known as drug-induced lupus, and this usually gets better when people come off the medication that caused it.
Lupus isn’t directly passed on from a parent to their children, but if you have a close relative with lupus then you may be at increased risk of developing it.
Lupus isn’t contagious, so you can’t catch it from anyone else.
How is lupus likely to affect me?
It’s difficult to say how lupus will affect you, because it can vary greatly between people who have it.
Treatments have improved a lot in recent years.
However, it is still a serious condition and can even be life-threatening in some situations when people’s vital organs are affected. But most people don’t have the serious complications.
If you have lupus, you will need regular check-ups with your doctors and nurses to look for any of the serious complications linked with the condition.
Because of the risk of serious complications, having a healthy diet and lifestyle, and exercising regularly is important.
If you have any new symptoms or concerns, talk to a member of your healthcare team.
Diagnosis
It can be difficult to make a diagnosis of lupus because it doesn’t affect any two people exactly the same. There are also many other conditions it resembles.
However, the earlier someone is diagnosed with lupus and treatment is started, the better their chances of keeping this condition under control.
A diagnosis of lupus is made based on symptoms, a physical examination and blood tests.
There are a number of tests that can help lead to a diagnosis of lupus or rule it out. These can then be used to monitor how well treatments are working. Some of these tests are:
Anti-nuclear antibody (ANA) test
About 95% of people with lupus test strongly positive for anti-nuclear antibodies (ANA), but the test can sometimes be positive in people who don’t have lupus, so it can’t confirm the diagnosis.
Anti-double-stranded DNA (anti-dsDNA) antibody test
About 70% of people with lupus have these antibodies. A positive test means that lupus is highly likely as the test is hardly ever positive in people who don’t have lupus. Levels of this antibody can go up as the lupus becomes more active and will go down if treatment is effective.
Anti-Ro antibody test
If you test positive for this antibody you may be more likely to get skin rashes and suffer from dry eyes or a dry mouth, known as Sjögren’s syndrome. Rarely, this antibody can pass across the placenta during pregnancy – this is the organ that passes food through from a pregnant woman to her unborn baby. If you carry the anti-Ro antibody and decide to have a baby, your pregnancy will be more closely monitored.
Antiphospholipid antibody test
A positive test for these antibodies may mean an increased risk of miscarriage and developing blood clots. These antibodies can come and go so these tests can be repeated.
Kidney and liver function tests
These include blood and urine tests, which are carried out regularly so any problems caused by the lupus or by drug treatment can be picked up and dealt with quickly.
A simple urine test can show if there’s protein or blood in the urine. This test can help doctors recognise a problem in the kidneys at an early stage. Further tests may be carried out if necessary.
Blood cell counts
Blood cell counts can help to show whether the bone marrow is affected, either by your condition or the drugs.
Scans and x-rays
Different types of scans and x-rays can assess how well your heart, lungs, liver and spleen are working.
Treatments
There’s no cure for lupus at present. However, the condition can respond well to a number of drugs. The earlier treatment is started, the more effective it’s likely to be.
Drugs
The drugs used to treat lupus will depend on how serious it is and which parts of your body are affected. Your treatments will probably be changed or adjusted as your symptoms flare up or improve. Many drugs used to treat lupus were originally developed for other conditions but were later found to be useful in lupus.
Non-steroidal anti-inflammatory drugs (NSAIDs)
These drugs can treat inflammation and pain in your joints. Examples include ibuprofen and naproxen.
They are often used for short periods of time. If used over a long term they can cause problems with the kidneys and so may not be advised for people who have had kidney disease. Other long-term side effects can include thinning of the lining of the stomach, so they may be prescribed with drugs known as antacids to protect against this.
You won’t usually be given NSAIDs if you’ve previously had stomach ulcers.
Steroids
Steroids, also known as corticosteroids, can reduce inflammation. There are different types of steroid medication.
Steroid creams can be used to treat skin rashes.
Tablets, for example prednisolone, can be used for short periods when symptoms are active. They can also be used as a longer-term treatment if symptoms persist, but will often be reduced to the lowest effective dose.
Steroid injections into a muscle or vein can help control a flare-up. Sometimes people can have steroid injections into the scalp to treat hair loss – though the hair often grows back on its own when the condition is brought under control.
When taking steroid tablets, it’s a good idea to carry a steroid alert card, which records your dose and how long you’ve been taking it. If you become ill, or have an accident and are injured or unconscious, it’s important for the steroid to be continued or possibly even increased. Steroid treatment can prevent your body producing enough natural steroids in response to a trauma such as an injury. Because of this it is important not to suddenly stop taking them if you have been on them for a while without speaking to your rheumatologist first.
Your doctor, rheumatology nurse specialist or pharmacist can give you a steroid card.
Antimalarials
These drugs can help reduce inflammation. They can help to lower cholesterol and control kidney conditions.
The most common example used to treat people with lupus is called hydroxychloroquine. It can be used alone or with steroid creams for skin rashes. It’s also useful for fatigue and joint pain.
In some cases, hydroxychloroquine can affect the eyes. While this is rare, it can be serious. Therefore, you will need regular eye tests if you are taking this drug – especially if you’ve been taking it for five years or more.
Disease-modifying anti-rheumatic drugs (DMARDs)
These are drugs that reduce the effects of an overactive immune system. This can stop the immune system having a damaging effect on the body’s own tissues. Examples include:
They may take several weeks or even up to three months to take effect. Then they might need to be taken over a long period. The dose could be reduced once your condition is under control.
They may be used along with steroid tablets and may allow the steroid dose to be reduced.
People on DMARDs will need to have regular blood testing to check how effective they are, and what impact they are having on the body.
Biological therapies
Biological therapies are a newer type of DMARDs. They have a more targeted effect on specific cells within the immune system. Examples include rituximab and belimumab.
They can remove or reduce the activity of B-cells. These are a type of white blood cells, and in people with lupus they may produce harmful autoantibodies that attack the body’s own tissues.
They can be used to treat people with lupus when older types of DMARDs aren’t effective or if the lupus is very active.
If you’re taking a biological therapy, it’s a good idea to carry a biological therapy alert card. You can get one from your doctor or rheumatology nurse specialist. If you become unwell, anyone treating you will know you’re on a biological therapy and that you’re therefore possibly at risk of its side effects, including infections.
If there’s a significant build-up of fluid in the lining tissues of the heart or lungs, this may need to be drained using a needle and syringe.
Rarely, some people with lupus develop kidney failure, which may require dialysis. This is a treatment to remove waste products and excess fluid from the blood when the kidneys stop working. In some cases, people may need a kidney transplant.
However, severe kidney damage can usually be prevented by early diagnosis and treatment of lupus.
What about side effects?
All drugs have some potential side effects, and you and your doctor will need to balance the risk of side effects with the need to control your symptoms. Sometimes this may mean taking additional medications to protect against the side effects of others.
Treatments such as calcium, vitamin D tablets and drugs called bisphosphonates may be given to guard against the bone-thinning condition osteoporosis. This condition can be a risk for people who take steroids at high doses or for long periods. You may be given DMARDs instead of high doses of steroids.
If you have lupus, and especially if you’re on a DMARD or biological therapy, you’ll be more prone to infection. Take care to avoid contact with people with infectious diseases like chickenpox or if they’ve recently been in hospital. You should discuss your vaccination status with your rheumatologist or GP. You might need to avoid live vaccines.
If you suffer from a severe infection or require antibiotics you may need to stop your DMARD treatment for a short time, and restart them once you’ve recovered from the infection.
Please visit our information pages on drugs for more information about your medication.
Self-help and daily living
Drugs are important in controlling lupus, but there’s also a lot you can do yourself to help manage your symptoms. Having a healthy diet, exercising regularly and not smoking will help reduce your risk of developing the more serious complications of lupus.
Managing a flare-up
Lupus is a condition that naturally improves and worsens at different times. Learning how to manage a flare-up of your symptoms helps you to be more in control of your condition.
The reasons for a flare-up can vary from person to person, but exposure to sunlight, too little rest time, infections and stress can all play a part. It can be useful to try to spot the things that lead to a flare-up and find ways of managing or avoiding them.
Keep in touch with your rheumatology team, especially through your rheumatology nurse specialist and the telephone advice line available in most units.
Fatigue
You may find you often experience fatigue, and it can be a big problem. If there’s a specific cause, such as anaemia or an underactive thyroid gland, this can be identified by a blood test and treated.
Some medications such as hydroxychloroquine can help. Learning to pace yourself – finding the right balance between rest and activity – will help. Exercise improves fitness and stamina and can therefore help in overcoming fatigue, but you’ll need to start gently and gradually increase the amount you do. Ask to see a physiotherapist for advice about suitable exercises.
Smoking
Many of the problems caused by lupus can be made worse by smoking. For example:
- Lupus and smoking can both cause narrowing of the blood vessels, causing circulatory problems and increasing the risk of strokes and heart attacks.
- Lupus can make you more at risk of infections involving your throat, airways or lungs. Smoking can cause long-term lung damage which can make these infections more frequent and severe.
- When lupus affects the kidneys it can lead to high blood pressure. Smoking can also contribute to high blood pressure, increasing the risk of strokes and worsening kidney disease.
While it can be difficult to stop smoking, treatments are available that can help you to stop. Talk to your GP or call a smoking helpline to find out the ways they can help.
If you do smoke, giving up can be one of the most important things you do to reduce the risk of the more serious complications of lupus.
Exercise
There will be times when you may not feel like doing very much and it’s important to rest when you need to. However, too much rest will cause the muscles to weaken and may make you feel more tired, so you need to find the right balance between rest and exercise.
Walking and swimming are recommended as they can improve fatigue, fitness, strength and stamina without putting too much strain on the joints. Even when you’re having a flare-up, a small amount of exercise is helpful, and you should find some gentle exercise that you can do even on a bad day.
Exercise, particularly weight-bearing exercise such as walking or jogging, can help to keep bones strong. This can reduce the chances of the bone-thinning condition osteoporosis, that can be more likely if you take steroid tablets.
Diet and nutrition
There’s only limited evidence available on the effect of diet in controlling lupus. However, there is some evidence that a diet low in saturated fat and high in omega-3, which is found in oily fish, may be helpful. You can also try taking fish oil supplements, but use fish body oil, not fish liver oil. Too much fish liver oil can cause you to have too much vitamin A, which can have side effects such as liver damage and hair loss.
Make sure to get enough vitamin D and calcium. These important nutrients are needed for strong bones.
Calcium is in dairy products, such as milk, cheese and yoghurts, as well as some green leafy vegetables.
In general, the best source of vitamin D is a healthy and safe amount of sunlight on bare skin. Because it isn’t possible to get enough vitamin D from sunlight all year round in the UK and because too much sunlight can be unhealthy for people with lupus, you might need to take vitamin D supplements.
Be careful of any exclusion diets where large food groups are removed from the diet – you need all the nutrients that a well-balanced diet will provide. Consult a dietitian if you need more specific advice.
Sunlight
Too much ultraviolet light from sunlight can cause a red rash across the cheeks and the bridge of the nose, often known as the butterfly rash. It can also sometimes cause problems with internal organs to flare up. Bear this in mind when choosing a holiday destination and discuss with your nurse specialist or dermatologist if in doubt.
Keep out of the midday sun and wear a hat. Keep your skin covered or use sun cream of factor 50 or greater – which is available on prescription for people with lupus. You can also buy high-factor sun creams that include a tint and can be used as foundation make-up. Be careful when sitting under sun umbrellas on a paved area as the sunlight will be reflected onto your face.
Raynaud’s phenomenon
If you experience Raynaud’s in your hands or feet, dress suitably for cold weather. Smoking is bad for the circulation and is likely to make symptoms worse. Regular exercise will improve your circulation.
There are also drugs that can be prescribed to people with Raynaud’s, to improve circulation to the fingers and toes. Talk to your doctor about these.
Looking after your mental health
Because of the pain, fatigue and disruption to life, lupus can cause anxiety and depression.
It’s important to talk to someone you trust if you’re feeling down or worried. This could be a friend, relative or a healthcare professional. Versus Arthritis has a helpline if you’d like to speak to one of our trained advisors. Our helpline is open Monday to Friday from 9am to 8pm. Call free from the UK on 0800 5200 520.
Even if it doesn’t affect the course of the condition, emotional stress can sometimes make lupus seem worse. It’s not always easy, but there are things we can all do to help manage stresses in our life. For example – you might want to try relaxation techniques such as meditation or mindfulness.
Your doctor may be able to refer you to a psychologist who can help with coping strategies.
Therapies such as cognitive behavioural therapy (CBT) may help. This is a talking therapy that can help you manage problems by changing the way you think and behave. It’s most commonly used to treat anxiety and depression, but can be useful for other mental and physical health problems.
Regular exercise can improve feelings of stress, anxiety and depression.
Work
If you have lupus, you may want to seek extra support at work. You could talk to your human resources department.
There might be equipment that your company could provide you with to make you more comfortable and help you do your job better. There may also be flexible working arrangements so you could work from home at least some of the week, or alter your shift patterns to avoid rush hours.
The Equality Act 2010 means that employers have a responsibility to remove barriers in the workplace for people with a disability and financial support is available to help them do this through the Access to Work scheme.
You may not think the term disability is appropriate for you, especially if your condition is well treated and under control a lot of the time. But it can apply to lupus, meaning you’re entitled to additional support to help you in your employment or education.
The Equality Act states that someone is disabled if they have a physical or mental impairment that has a substantial and long-term negative effect on their abilities to do normal everyday activities, if they weren’t taking any medication. It might help to ask yourself, if I wasn’t taking any medication, would I find it difficult to do things such as dress or wash myself, go shopping or go out to work on my own?
Meeting others with lupus
Lupus is a difficult condition to live with and throws up many challenges, especially during periods of life when you may need more energy.
Meeting others with lupus doesn’t necessarily remove these challenges but it can help you to cope with them by sharing your thoughts and concerns with someone who understands. You may have access to an education programme through a lupus nurse specialist or you may wish to meet others through patient support groups such as LUPUS UK.
Contraception
If you have lupus you should talk to your doctor about what form of contraception would be best for you. It can be important to avoid unplanned pregnancies if you have lupus, particularly when your condition is active and affecting your kidneys, if you’re on certain drugs, or if you have high blood pressure.
You might need to avoid contraceptive pills containing oestrogen as there is a very small risk that they can cause blood clots, known as deep vein thrombosis (DVT). These blood clots can be dangerous if they break off and travel around the body, such as to the lungs.
This is more of a risk if you have antiphospholipid antibodies, which means you’re already at risk of blood clots.
It’s best to use contraceptive pills that contain only progesterone or only low-dose oestrogen, or consider barrier methods of contraception, such as condoms.
If you’re taking steroid treatment, you should avoid using the contraceptive medroxyprogesterone acetate, which has the trade name Depo-Provera. This is given by injection. It increases the risk of developing osteoporosis because it reduces the levels of oestrogen in your body, which is important for bone health.
The Mirena coil, which releases progesterone only, is often a recommended option for women with lupus.
Hormone replacement therapy (HRT)
In the past there has been concern about hormone replacement therapy (HRT) increasing the risk of flare-ups of lupus. However, recent research has suggested that it’s relatively safe to use for short periods if symptoms of the menopause are severe and your lupus is otherwise well controlled. Make sure you speak to your rheumatologist if you are planning to start HRT.
Complementary medicines
There’s no scientific evidence that suggests any form of complementary medicine helps to ease the symptoms of lupus. But if you have joint pain, acupuncture and massage may help. The pain relief may only last a short time to begin with, but repeated treatments may bring longer-lasting benefits. You may need to visit a private practitioner as the treatment may not be available on the NHS.
Generally speaking, complementary and alternative treatments are safe if you want to try them, but you should always discuss their use with your doctor before starting treatment. There are some risks associated with specific therapies.
In many cases, the risks associated with complementary and alternative treatments are more to do with the therapist than the therapy. This is why it’s important to go to a legally registered therapist, or one who has a set ethical code and is fully insured.
If you want to try a complementary or alternative treatment, it’s important to talk to your doctor first.
Pregnancy and lupus
Most women with lupus should be able to have a baby if they wish to. It’s best to discuss your plans with your doctor before trying to get pregnant so your treatments can be altered if they need to be. You may need to see an obstetrician with a special interest in lupus for further advice.
The following drugs must be stopped before you get pregnant, because they can harm an unborn baby:
You might also need to wait for a period of time after coming off any of these drugs before it is safe to get pregnant. If you become pregnant unexpectedly while on one of these drugs, talk to your healthcare team as soon as you can.
In contrast, steroids, hydroxychloroquine and azathioprine are safe to take during pregnancy.
If you can, it’s best to try for a baby when your lupus is not active.
A small number of women with very severe lupus may be advised against having a baby as pregnancy can put a strain on the heart, lungs and kidneys. There’s an increased risk of pregnancy complications in women whose lupus affects a number of different organs and who find it difficult to control their symptoms without certain medications.
There are also restrictions on drugs that you can take if you’re breastfeeding. Talk to your rheumatology team or GP.
If you have high levels of antiphospholipid antibodies there’s an increased risk of miscarriage. However, treatment with aspirin or heparin reduces this risk, and there are now many more successful pregnancies in women who have these antibodies.
There’s conflicting evidence about whether pregnancy is likely to cause a flare-up of lupus. If your condition is well controlled at the time you became pregnant, and you don’t have kidney disease, then you’re unlikely to have any problems.
If you do have kidney disease, you may have increased protein in your urine during the later stages of pregnancy. Protein in urine could also be a sign of a condition called pre-eclampsia. This causes pregnant women to have high blood pressure and it is more common than kidney disease. If you have proteins in your blood during pregnancy it can be difficult to work out whether this is due to kidney disease or pre-eclampsia. The doctors looking after your pregnancy will check for this and consult your rheumatologist if necessary.
In pregnant women who have anti-Ro antibodies there’s a small risk that their babies will have neonatal (newborn) lupus syndrome. This means the baby may have a rash or a slow heartbeat. If this happens in one pregnancy, there is a slightly greater risk that it could happen in any further pregnancies. Most babies born to mothers with anti-Ro antibodies will be fine, but it’s important to have regular scans of the baby’s heart during the pregnancy.
Research and new developments
Versus Arthritis supports a wide range of projects that aim to prevent the onset of lupus, transform its treatment and ultimately find a cure.
New therapeutic approaches that target cells and molecules believed to be part of the cause of lupus are being used to help many patients. Further research studies should allow us to find out how these and other drugs can be used to the best effect.
We’re currently funding research into many aspects of lupus, for example:
- A study, being carried out at University College London, is looking into the potential link between a lack of iron in the blood and fatigue in lupus patients. This could lead to the development of new treatments to combat fatigue.
- Research is investigating how messaging molecules influence the response produced by the body to rituximab. This could lead to new treatments.
- A pilot study is investigating if a medication called belimumab can be used to prevent relapses after rituximab therapy. This could eventually provide a new treatment option for lupus patients.
- Research is looking at why vascular disease often develops in people who have lupus. This could lead to the development of new drugs that could reduce the risk of heart attack or stroke in lupus patients.
- Research is helping us to understand how changes in a specific gene contribute to the risk of developing adult lupus, and which genetic factors lead to the development of lupus in children. This could help develop new treatments for children and adults.
Anthony’s story

I was diagnosed with discoid lupus over 20 years ago. It started with a spot on the tip of my nose and rashes and discolouration on my face, including my eyebrows.
One day a hairdresser asked if I’d ever had brain surgery because of the dark discoloration to my scalp. I also had indents on my fingertips. I was in my mid-twenties and didn’t understand what was happening.
For a time, I was successfully managing my discoid lupus, thanks to being prescribed hydroxychloroquine.
But four years later I started developing new symptoms. It began with night sweats, my bed clothes would be soaked. My sense of smell altered.
I’d go to work, come home, feel so tired, and need to sleep for a couple of hours. I’d then wake up, have a shower and go to bed for the night. I couldn’t do anything in the evenings.
I couldn’t sleep flat. I had pillows to prop me up. My GP sent me to A&E, and this led to a diagnosis of pleurisy – inflammation around the lungs.
After being in hospital for a week I was off work and recovering at home. I was coming to the end of 10 days on ibuprofen when one day my feet were so painful I couldn’t put any weight on them. I then started to develop joint pains everywhere.
The slightest movement was extremely painful and I was really struggling.
Because of all these new symptoms I was referred to a rheumatology consultant, who confirmed I had developed SLE. This was a scary and bewildering time.
I was tried on different kinds of immunosuppressive drugs, and I eventually settled on methotrexate. I was also prescribed steroid tablets as well as calcium with vitamin D. I was still taking the hydroxychloroquine.
It then came to light that I was developing issues with my kidneys and so I was put on a drug called mycophenolate mofetil, and I was taken off methotrexate. The real plus for me was this resolved my joint pains.
As I had been on hydroxychloroquine for a long time, last year my rheumatologist stopped prescribing me it due to concern about the risk to my eyes.
I’ve always believed in the importance of good nutrition and exercise.
I wasn’t going to allow my condition to stop me exercising. It’s so important to keep your body mobile and fit. Exercise doesn’t just help physically, but also emotionally and psychologically.
With lupus, there can be confusion, frustration and resentment. But you have to try to understand, accept and even embrace what’s happening, before you can move forward.
My advice would be keep on top of your medication, have a healthy lifestyle, try to understand your condition and make the most of the expertise, care and help available from your healthcare professionals. It’s important to have a good relationship with your clinicians, but also to take responsibility for yourself.
I’m thankful that the management teams at my places of work have been understanding when issues of my lupus have arisen.
Generally, my lupus doesn’t stop me working or enjoying my hobbies.
Have positivity and hope in your armoury. There is always hope, there is always help available, and you will have possibilities and options open to you.
Monique's story

When I was 25 I went to see my family in the Caribbean. This was a trip I regularly made and loved going on. But it was soon clear things weren’t right. I was depressed, I’d lost my appetite, and my energy levels were low.
My relatives were concerned and took me to a hospital for some tests, but nothing was discovered.
One day we went to the cinema and I became very unwell. When the movie was finished, I couldn't put my feet on the ground, I was in excruciating pain. It was like pins and needles multiplied by 1,000 times. I had to be carried out of the cinema. It was scary.
This was back in 2007 and shortly after I got home to London, I went to my local hospital for further tests. This led to a diagnosis of lupus.
I remember thinking, 'How can I get this? I'm young, fit and healthy'. It was a big adjustment for my family and I.
A major problem over the years has been fatigue. I have to plan the week ahead. Fatigue is always there. Sometimes you don't have to be doing much and you get this overwhelming need to sit or lie down.
I try to sleep and eat properly. I've cut out red meat and swapped it for fish, chicken and vegetables. I also drink lots of water.
Last year I returned to work after some time off because of my lupus. I work for the Deaf and Disabled People’s Organisation (DDPO).
I was quite anxious going back to work. I am confident and outgoing, but I found it quite daunting. My body is different from my pre-lupus days.
Through the Access to Work scheme I was provided with an adjustable chair and desk, and this made the world of difference.
It helps to be open about your condition, so you can get the support you need and are entitled to. Being open and talking about my condition has been a positive for me.
I set myself SMART goals. This stands for specific, measurable, achievable, realistic and time bound. So I used this when thinking about what jobs to apply for, location of workplaces, hours I could work a week.
It’s important to push yourself a bit, but not too much so that it’s not possible.
It has taken me 13 years to reach this point; and it has not been easy. Returning to work has been a personal achievement for me, and for many returning to work is not an option due to their condition and the symptoms.
I am still very much a work in progress and after 13 years I am still discovering the limitations of my body because of lupus and arthritis. If my journey gives one person hope that their situation can change, given time, I would be happy.