What is systemic sclerosis (scleroderma)?
Systemic sclerosis is a rare condition that can cause people’s skin and the connective tissue inside the body to harden.
You can sometimes see signs of systemic sclerosis on the face, hands, feet and elsewhere around the body, as skin hardens and thickens.
Systemic sclerosis can also cause connective tissue inside the body to become thick and hard.
Connective tissue includes tendons, cartilage and blood vessels. Together they form a structure that supports joints and internal organs, and holds them in place.
When skin and connective tissue hardens and thickens it becomes like scar tissue from an injury or a burn. When systemic sclerosis causes connective tissue to harden this can stop muscles, blood vessels, joints and internal organs such as the lungs, working as well as they should.
Most people with systemic sclerosis will only have mild symptoms. Rarely, it can cause serious problems with internal organs. These complications can be treated.
It’s important that potentially serious complications are spotted early. You should therefore have regular check-ups with your doctor, preferably once a year.
Systemic sclerosis is an autoimmune condition. This means that the immune system, which protects you from illness and infection, gets confused and attacks the body’s own cells.
The word systemic means a condition that can affect the whole body. Sclerosis means the hardening of a structure.
Systemic sclerosis affects more women than men. It usually starts between the ages of 25 and 55, although it can occasionally start in children or in older people.
There are different types of systemic sclerosis – diffuse and limited.
Diffuse systemic sclerosis can affect skin all over the body and is more likely to affect the internal organs.
Limited systemic sclerosis is a milder form that only affects the skin on the face, lower arms, hands, lower legs and feet. It normally progresses slowly. Limited systemic sclerosis can affect the lungs and the digestive system too.
Systemic sclerosis is not to be confused with a separate condition called localised scleroderma, which just affects the skin. The word scleroderma, which is an older term, specifically means hard skin.
The following information is about the condition systemic sclerosis, in which skin and connective tissue inside the body are affected.
Symptoms
Systemic sclerosis can cause symptoms affecting different parts of the body.
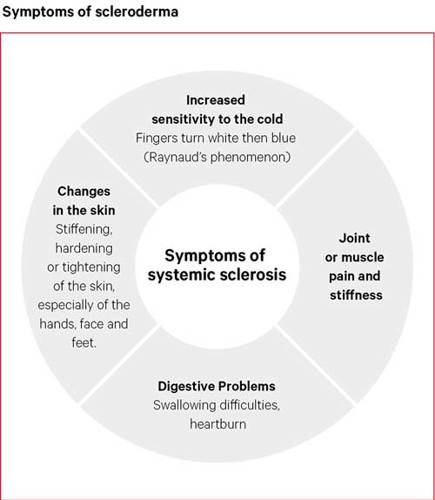
Sensitivity to the cold (Raynaud’s phenomenon)
Most people with systemic sclerosis develop an unusual sensitivity to the cold, known as Raynaud’s phenomenon.
Fingers or toes turn white then blue in the cold. Just walking into a cold room or reaching into a fridge or freezer can make this happen. The colour returns to normal as the hands or feet warm up.
Raynaud’s phenomenon is caused by a narrowing of the blood vessels, which reduces the blood supply to the fingers or toes. Stressful situations can also cause the blood supply to reduce in the hands and bring on an episode of Raynaud’s.
Many people have Raynaud’s without ever having systemic sclerosis. However, most people with systemic sclerosis will have symptoms of Raynaud’s at some time during their illness.
Raynaud’s is often the first sign that someone has systemic sclerosis. It can sometimes appear years before the onset of systemic sclerosis.
Changes in the skin
The most common changes in the skin due to systemic sclerosis are:
- thickening and hardening of the skin on the hands, arms and face
- swelling of the hands and feet, especially in the morning
- shiny skin, without its usual creases
- stiffening of the facial skin, making it difficult to open the mouth wide
- small red blood spots on the face, hands and arms.
Less frequently, or later on in the condition, there may be:
- thinning of the lips
- thinning of the skin on top of the fingers and the soles of the feet
- peeling, cracking or open sores (ulcers) in the skin and flesh over the fingertips, caused by poor blood supply
- white chalky lumps under the skin, caused by deposits of the mineral calcium, often on the fingertips.
Digestive problems
Systemic sclerosis can affect the digestive system, which is responsible for swallowing food, breaking it down, and sending it to different parts of the body.
We have a tube that takes food from the mouth to the stomach, called the oesophagus (o-soff-a-gus). Systemic sclerosis can cause the muscles in this tube to weaken, which can make swallowing difficult.
Systemic sclerosis can cause heartburn, as a result of too much gastric acid in this food tube. This acid is produced naturally in the stomach to help break food down.
However, systemic sclerosis can cause this acid to leak upwards from the stomach into the food tube. This can be unpleasant, and it isn’t good for us.
Most people with systemic sclerosis have some problems with swallowing or heartburn. Less often, other parts of the digestive system may be affected, leading to bloating, diarrhoea or constipation.
Pain or stiffness in the joints or muscles
Systemic sclerosis can cause the tissues around joints to stiffen, which can reduce the range of movement of joints.
It can also cause pain and swelling around affected joints.
Muscle weakness is also sometimes a symptom of systemic sclerosis.
People who have had systemic sclerosis for a long time may find that their joints can tighten into a bent position, because of the tightening of the skin and tissues surrounding the joints.
How is systemic sclerosis likely to affect me?
Systemic sclerosis affects everyone differently, so it’s hard to say how it might affect you.
This is a long-term condition, however the serious problems it can cause are rare.
About one in five people with systemic sclerosis will also have symptoms of another condition, such as lupus, Sjogren’s syndrome or inflammatory arthritis. These conditions will also need treatment.
Most people find that systemic sclerosis affects just a few parts of the body and comes on gradually. It may slowly get worse but usually settles down to become stable after a few years.
Sometimes systemic sclerosis may progress more quickly.
For some people the symptoms can almost disappear after several years.
The skin symptoms can be the worst part of systemic sclerosis for some people. While for other people, the digestive problems will give them the most problems.
Unfortunately, systemic sclerosis can sometimes cause people serious problems. These can include:
- scarring of the lungs, causing shortness of breath and a dry cough
- narrowing of the blood vessels of the lungs, leading to high blood pressure in the lungs, which may in turn strain the heart
- kidney problems resulting in high blood pressure.
These problems are rare. However, it’s important you have regular check-ups with your doctor – preferably once a year – if you have systemic sclerosis.
The body is able to break down or repair extra scar tissue. This means there may be some improvement in scarring – both in the skin and in other organs – once it becomes less active.
Diagnosis
There’s no single test for systemic sclerosis, and often it’s the thickening of the skin that will be a key reason why a doctor has made a diagnosis.
However, your doctor will carry out tests that can be helpful in finding out whether other parts of the body are affected.
What tests are there?
Tests could include:
- blood tests
- x-rays and computerised tomography (CT) scans
- breathing tests
- a heart scan, for example an echocardiogram
- stomach tests, (for example an endoscopy)
- a skin biopsy, where a small piece of skin is removed and examined under a microscope
- a capillaroscopy, which looks at the small blood vessels (capillaries) around the finger nails that are often affected by systemic sclerosis.
Infrared thermography uses technology to take images of what’s happening inside the body by showing heat spots. This can be used to help make a diagnosis of systemic sclerosis. These tests are often only performed at specialist centres.
Treatment
There’s currently no cure for systemic sclerosis. However, there are drugs that can help to control symptoms and treat any complications.
There are many ways systemic sclerosis can affect the body. Therefore, the treatment you’ll need will depend on how the condition affects you.
There’s also a lot you can do to help manage your condition, including regular exercise, a healthy diet and a good skin care routine.
Treating Raynaud’s phenomenon
Drugs can help with the symptoms of Raynaud’s phenomenon by improving circulation to the hands and feet.
There are quite a few drugs available that can have this effect, including nifedipine and sildenafil, which can be taken as tablets. You may need to take more than one drug at the same time.
In more severe cases of Raynaud’s, particularly where there are painful ulcers that won’t heal, drugs such as iloprost can be given as an infusion. An infusion is a way of giving a drug as a drip into a vein, usually in a hospital.
Drugs to treat Raynaud’s phenomenon work by relaxing the blood vessels and increasing blood flow to the fingers and toes. They will also have the same effect on blood vessels elsewhere in the body. Therefore, these drugs can cause side-effects such as skin flushing, headaches and swelling of the ankles.
Treating heartburn and swallowing difficulties
To prevent heartburn and swallowing difficulties, your doctor may recommend antacids, a type of medication that can neutralise the acid produced in the stomach.
These are usually very effective, although you may need to take them for months or years.
You may also be prescribed a drug called a proton pump inhibitor (PPI), which can reduce the amount of acid produced by the stomach.
Treating other problems related to the stomach and digestive system
If you have spells of constipation and diarrhoea, abdominal swelling, increased wind and discomfort, you may need to see a gastroenterologist who specialises in this area.
Some people also experience anal incontinence, meaning that they can’t control their bowel motions properly so that small amounts of stool slip out and can soil their clothes.
This can be uncomfortable or embarrassing, and people may not realise that it’s anything to do with systemic sclerosis. If this happens to you, talk to your doctor and ask for a referral to a gastroenterologist.
Sometimes additional bacteria develop in the bowel, and this can be treated by drugs such as antibiotics.
It’s important to have symptoms like diarrhoea and incontinence looked at, to make sure that they don’t have another cause.
Treating painful and swollen joints
Painkillers and non-steroidal anti-inflammatory drugs (NSAIDs) should help to relieve joint pain and swelling.
You can buy milder forms, such as paracetamol and ibuprofen, over the counter at pharmacies and supermarkets. Your doctor will be able to prescribe stronger painkillers and NSAIDs if needed.
Treating high blood pressure and kidney complications
People with systemic sclerosis can sometimes have high blood pressure, also known as hypertension. Severe cases can lead to kidney damage and strain on the heart.
This is a serious complication known as a systemic sclerosis renal crisis. It can be treated or prevented with drugs that help to control the blood pressure, especially ACE inhibitors.
Treating lung and heart complications
Inflammation in the lungs can be treated with steroids or disease-modifying anti-rheumatic drugs (DMARDs).
High blood pressure in the lungs (pulmonary hypertension) is a rare complication of systemic sclerosis, but you’ll have regular tests to check how well your lungs and heart are working.
If necessary, pulmonary hypertension can be treated with specific drugs (including bosentan, ambrisentan, sildenafil or prostacyclin) that improve symptoms such as breathlessness.
Other drugs that may be used for lung and heart complications include:
- steroid tablets
- drugs to suppress an overactive immune system
- drugs used to treat blood pressure and cholesterol.
Steroid tablets to treat systemic sclerosis
Steroid tablets can be used either in the early stages of systemic sclerosis when the skin is starting to look puffy, or later on if the muscles or lungs are affected.
They’re usually given in low doses because high doses can raise blood pressure and increase the risk of kidney problems.
Steroid tablets are man-made forms of a hormone (cortisone) that occurs naturally in the body. They can be used to reduce swelling.
Immunosuppressive drugs to treat systemic sclerosis
Immunosuppressive drugs target the immune system and may be used in more severe cases of systemic sclerosis, especially where the skin or lung disease is more extensive.
These could include drugs which are known as conventional disease-modifying anti-rheumatic drugs (DMARDs).
These drugs which have the effect of reducing the effectiveness of an overactive and misfiring immune system, include methotrexate, ciclosporin, cyclophosphamide, mycophenolate and azathioprine. It will depend on how systemic sclerosis affects you as to whether you will be prescribed any of these drugs.
The biological therapy rituximab is sometimes used to treat severe cases of systemic sclerosis. Biological therapies are newer drugs that have a more targeted approach. They reduce the effectiveness of key cells in the immune system that may be causing problems.
Living with systemic sclerosis
For some of the symptoms of systemic sclerosis you will need to take drugs. However, a healthy and balanced diet, exercising regularly and a good skin care routine are also important.
Exercise
A regular exercise programme will keep your skin flexible, reduce any tightening in your joints and keep your blood moving freely.
Although you may need to rest if your joints become swollen, it’s generally helpful to keep moving as much as possible.
Regular stretching and range of movement exercises, should help to reduce tightness around the joints, particularly in the hands and wrist.
A physiotherapist or a specialist hand therapist would be able to teach you the best exercises to keep your joints mobile. They may also suggest using splints to wear to help you look after your hands and wrists.
A physiotherapist might be able to give you special exercises to help maintain mobility in the muscles, connective tissue and skin in your face.
Diet and nutrition
Maintaining a healthy diet is important as it may help Raynaud’s symptoms and the healing of skin ulcers.
However, digestive problems can make it difficult to keep up a balanced diet and to keep to your normal weight.
If you have heartburn or difficulty in swallowing, the following tips may help:
- Eat six small meals a day instead of three larger ones. This helps with digestion, while making sure that your body gets the nutrients it needs.
- Eat slowly, chew thoroughly and drink plenty of water with meals.
- Eating your largest meal in the middle of the day can help to avoid heartburn.
- If you suffer with heartburn, see your doctor, who may prescribe a proton pump inhibitor (PPI) that will help to reduce irritation of the gullet.
- Don’t eat too much in the evening to make sure you have time for digestion before you go to bed.
- Raise the head of your bed a few inches to stop acid coming back up from your stomach while you sleep.
Complementary medicine
Massaging the hands using warm paraffin wax can help to keep the skin flexible and reduce discomfort in your joints. However, you must not use a wax bath if you have any open finger ulcers.
While there is a lack of scientific evidence to say that complementary medicine can help ease the symptoms of systemic sclerosis, most are thought to be safe to use. It’s always important to go to a reputable and registered supplier. It’s also very important to check with a GP first if you think you’d like to try a complementary medicine.
In many cases the risks associated with complementary and alternative therapies are more to do with the therapist than the therapy itself. This is why it’s important to go to a reliable and legally registered therapist, or one who has a set ethical code and is fully insured.
The use of high-dose vitamins E and C, fish oil and ginger or gingko dietary supplements can also help. If the vitamins don’t help within a three-month period, you should stop taking them.
Always talk to your doctor before you try a complementary medicine.
Supports, aids and gadgets
If you have trouble with daily activities like dressing or tasks that need you to have good grip strength, there are a number of gadgets available that can help. If in doubt, ask an occupational therapist for advice on how to protect your joints from unnecessary strain.
If you struggle to open child-proof medicine containers, ask your pharmacist to put your drugs in containers you can manage.
Some people find it difficult handling coins when their fingers are sore or swollen. A coin purse that opens out to form a tray for the coins may help with this.
If you think that an aid or gadget might help you with a task you’re struggling with, the charity Remap might be able to help you. This organisation makes bespoke equipment free of charge for people with a medical condition to help them with essential daily tasks.
If you live in England, and have systemic sclerosis, you may also be entitled to free support from your local authority to help with everyday tasks and getting around your home.
You could get help with the costs of aids and minor adaptations if you meet eligibility criteria. The criteria includes that you have a physical or mental illness or disability, and are unable to do basic tasks or activities, such as:
- cooking
- eating
- washing
- going to the toilet
- getting dressed
- cleaning
- working
- developing and maintaining family and social relationships
If you’re unable to do two or more of the above tasks or activities, and this has a significant impact on your well-being, you should qualify for aids and minor adaptations.
If you are eligible, you should be able to get aids, and minor adaptations up to the value of £1,000 per item, free of charge. If you need an adaptation which will cost over £1,000 you can apply for a disabled facilities grant. All these aids and adaptations can help with everyday tasks around your home and make it easier to get around.
For more information, visit this website for a needs assessment: www.gov.uk/apply-needs-assessment-social-services
Skin care and keeping warm
You need a good supply of blood flowing to your skin to stop it from cracking, peeling and developing ulcers.
Here are some things you can do to help:
- Keep warm from top to toe – this will help open the blood vessels to your arms, hands, legs and feet. Wear a hat to help preserve your body heat. Thermal clothes, hand warmers and electrically heated gloves and socks can also help. Remember that layers of clothing will trap heat and keep you warmer than thick clothes.
- If your skin is broken or painful, dressings can help to protect it.
- Don’t use strong detergents or anything else that irritates your skin, and avoid soaps that contain the natural wax lanolin.
- Try soaps, creams and bath oils designed to prevent dry skin until you find the ones that give you the best results in keeping your skin supple.
- If your hands are prone to dry skin, put cream on them whenever they’ve been in water. You can use either a water-based cream (such as E45 or aqueous cream), which is short-acting, or an oil-based cream (such as emulsifying ointment), which is thicker and longer-lasting.
- Smoking reduces the blood flow to your skin and is very likely to make Raynaud’s symptoms worse, so it’s best not to smoke. If you need help to stop smoking, talk to a GP or pharmacist, who will be able to offer support and advice. They may also be able to refer you to a local Stop Smoking service.
Managing red blood spots (telangiectasia)
Telangiectasia are small red spots on the skin that often develop on the face, hands, and sometimes the chest and arms. They don’t cause any harm.
They are caused by blood vessels becoming wider than normal.
You can use make-up to help cover them up if you want to, which shouldn’t make your skin symptoms worse.
Changing Faces, a charity for people with conditions, marks or scars that affect their appearance, offer a skin camouflage service, giving advice on how to cover the marks with camouflage cream.
Clinics are available throughout the UK and you can find information on the nearest one to you by visiting their website, www.changingfaces.org.uk.
The service is free (though donations are welcome) and is open to anyone. Changing Faces accept self-referrals in some areas, but in others you’ll need to get a healthcare practitioner to refer you online.
Laser treatment can also help in some cases. It’s available in the specialist dermatology units of some hospitals, and you may need several sessions to keep the telangiectasia under control.
Dealing with stress
There may be emotional difficulties connected with having a long-term condition, and the changes in the appearance of your skin can be upsetting. In addition, stress can reduce the blood flow to some parts of your body, so it can affect your condition, particularly if you have Raynaud’s phenomenon.
Talk about any feelings of stress or depression with your family, friends or a healthcare professional. If you need help in handling stress or depression, your doctor may be able to help or can refer you for specialist counselling.
You can also speak to a nurse in the rheumatology clinic. Many clinics have nurses who either specialise in systemic sclerosis or have a special interest in the condition.
Another option could be to get in touch with Scleroderma Raynaud’s UK (SRUK), a charity that provides services to people with systemic sclerosis and Raynaud’s phenomenon. This is a members’ organisation and it provides a range of support services. Talking to people with the same condition can greatly help.
Related information
Research and new developments
Versus Arthritis is currently funding several studies to improve our understanding of the causes of systemic sclerosis.
This includes a long-term study to find out whether a new light-based imaging technique can be used to measure different features of the condition.
This technique has potential to tell us more about what causes blood vessel narrowing and tissue scarring (fibrosis). It may also lead to research into new therapies for systemic sclerosis.
We’re also supporting research to better understand what causes excessive scarring of the skin and internal organs in people with systemic sclerosis. Scar tissue is made by cells called myofibroblasts, and a protein called c-Rel is thought to regulate its production. This research aims to understand how c-Rel regulates scar production and to discover whether altering its function or removing it will prevent scar formation.
We’re also funding research to identify new treatments for systemic sclerosis, including a study which aims to investigate whether treatment with the steroid prednisolone is beneficial, in terms of safety and effectiveness, in patients with the condition.
Barbara’s story

My symptoms started in July 2013. My fingers were swelling up like crazy, and my ankles were swelling up so much I couldn’t see them. No-one could tell me what was going on. I was referred to a rheumatologist.
Nothing was showing up in my bloods to indicate anything in particular. But over the following few months, more and more started to go wrong.
I was having trouble walking and I was out of breath all the time. The walk from my car to work was too much, so my husband would drop me off right at the door. After Christmas, I had another blood test and something showed up.
The rheumatologist said: ‘I think we have to put you on some immunosuppressive drugs.’
We went on a skiing holiday in northern Italy, and because it was at high altitude that set things off. I became ill and was struggling to breathe. I had to be helicoptered to a hospital in a town called Bolzano.
I was in this hospital in Italy for two-and-a-half weeks. It was there a doctor said: ‘Has anyone ever told you that you have scleroderma?’ I’d never heard of it before. It was quite a shock. They got me stabilised, so I could come back to England.
I came back to the local hospital and was transferred to a renal unit in Manchester. I had a serious problem with my kidneys.
They did a biopsy on my kidneys and took me off my medication. I was there until they confirmed that fortunately I didn’t need a kidney dialysis. When they saw signs of improvement, I was allowed home.
I have good days and bad days. On a bad day, I’m very tired and don’t want to do anything, and there can be pain. One of the biggest ways it has affected me is my skin. It has made my skin extremely tight, and it gets shiny, itchy and painful. My skin is almost normal again now.
My treatment was quite aggressive early on, but it seemed to have the desired effect. I had to give up work though. I was too ill to continue at the time.
It is easy to say, and difficult to do, but you have got to keep a positive mindset that you will get through the worst of it.
This is a tough condition, and if you’re prone to depression, this can make it worse. What really helps, is to talk to people. It helps if you have a good supportive family around you, and I am lucky to have that.
My husband Andrew and I get out for a walk on a daily basis. If I’m sat around for too long, I stiffen up. And just being out in the fresh air, is good for the mind.