How our research is improving care for rare conditions like vasculitis
29 February 2024
Navigating the healthcare system can be challenging when you’re living with a rare condition, such as vasculitis.
What is vasculitis?
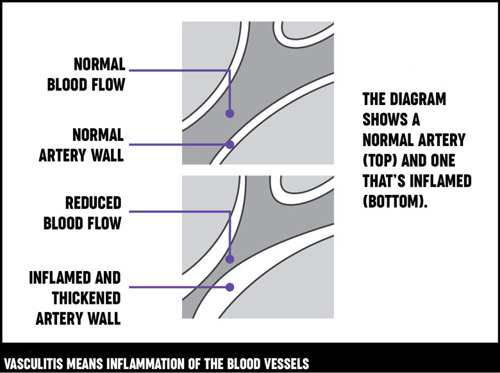 Vasculitis is a group of rare inflammatory conditions that cause inflammation of the blood vessels. These are the tubes that carry blood around your body, such as your veins, arteries, and capillaries. Any blood vessel in your body can be affected by the condition.
Vasculitis is a group of rare inflammatory conditions that cause inflammation of the blood vessels. These are the tubes that carry blood around your body, such as your veins, arteries, and capillaries. Any blood vessel in your body can be affected by the condition.
There are different types of vasculitis, and it can lead to problems that can be mild, severe, or even life-threatening.
Even people with the same type of vasculitis can be affected in different ways and need different care.
While vasculitis is not curable and can keep coming back, it can be controlled using medicines. So, diagnosing and treating the condition early is important to prevent damage to the body.
Learn more about vasculitisDiagnosing and treating vasculitis
Vasculitis isn’t easy to diagnose. As well as being rare, it can affect many different parts of the body such as the:
- kidneys
- heart
- lungs
- nerves
- ears
- eyes.
Because of this, it can lead to symptoms that can easily be confused with other conditions. People living with vasculitis often need care from lots of different specialists too.
For these reasons, it can sometimes be difficult for people living with vasculitis to get the care and support they need.
What did the researchers want to find out?
We wanted to understand what good care looks like for people living with vasculitis and how we can put this into practice.
So, our researchers at the Aberdeen Centre for Arthritis and Musculoskeletal Health set up the VOICES (Vasculitis Outcomes In relation to Care ExperienceS) study to tackle this.
They worked together with people living with vasculitis and healthcare professionals to learn:
- About their experiences living with and looking after people with vasculitis.
- About the barriers they face when accessing care, and the difficulties of delivering services.
- How healthcare can be made better for people living with vasculitis.
This study focused on primary systemic vasculitis.
‘Primary’ means that the vasculitis isn’t a result of another illness, such as rheumatoid arthritis. ‘Systemic’ means it can involve any part of the body.
Read more stories about our researchWhat did the researchers do?
In this study, our researchers looked at numerical data and non-numerical data such as interviews. This is sometimes called a ‘mixed-methods study.’
Using surveys and interviews, the researchers heard from people living with vasculitis and healthcare professionals about their healthcare experiences.
They looked at how vasculitis care is delivered across the UK and Ireland. To do this, they analysed health data that is routinely collected, for example, when you stay in hospital.
“Different groups' perspectives have been listened to, and so this study has for the first time given a clearer picture of what patients are experiencing regarding access to treatment and support services and more importantly suggestions on what and where improvements could be made.”
What is the VOICES patient and public involvement group?
People living with systemic vasculitis were also members of the VOICES patient and public involvement group.
These are groups of patients who act as ‘partners’ rather than participants in research. They:
- Helped to design the study, analysed the information collected, and reflected on the findings.
- Presented at conferences.
- Helped develop recommendations for healthcare practice.
- Wrote about the importance of patient and public involvement in research.
- Created online resources for people with vasculitis, including filmed stories from people living with vasculitis. By hearing other people’s experiences, we hope it might help people living with rare diseases feel less alone.
“The VOICES study has for the first time provided evidence of how best to deliver effective services that will improve outcomes and experiences of care for people living with vasculitis,” says Rosemary Hollick, Chief Investigator, VOICES study.
“This information is already being used to inform clinical service standards, guidelines and policy, and strategies to overcome the barriers to achieving this in practice.”
Charlie's story: Navigating healthcare
What did the researchers discover?
Through carrying out this study, the researchers found:
- Good care for people with vasculitis is when healthcare teams:
- respond to illness quickly (including getting a diagnosis, providing urgent treatment and flare-ups of the condition).
- provide continuity of care (seeing the same clinician, team and sharing of information across different teams).
- support people to make decisions about their care (shared decision making).
- Practical changes to healthcare which would help people living with vasculitis include:
- Timely access to services: When a new patient with suspected vasculitis waits less than a week for a consultation, and there is a nurse advice line for patients, there are fewer serious infections and emergency admissions. A nurse advice line is a dedicated telephone line for patients to access advice about their condition.
- Coordinated healthcare: When a patient is treated in a healthcare setting alongside people with similar conditions or needs (sometimes called ‘a cohorted clinic’), and there are clinics led by nurses, there were fewer serious infections and emergency admissions to hospital.
- Access to the right expertise: When a patient’s healthcare team regularly host meetings with the different healthcare professionals involved in their care (multi-disciplinary team meetings), it improves communication and co-operation. It also gives patients the chance to be more involved in their care.
- Delivering healthcare in this way helps healthcare teams work better together and makes people living with vasculitis feel safer.
- Access to key service components varied across the UK and Ireland, particularly access to nurse led care and vasculitis multi-disciplinary team meetings.
The researchers also discovered many barriers when trying to put these healthcare suggestions in place. For example:
- The different specialities involved in looking after people with vasculitis work in very different ways and were often not used to working together.
- Services providing care for people with vasculitis were often not aware of care offered by other specialties. This made it difficult to ‘join up’ care.
- There are no standards to guide what services should be in place, or measures (audits) of what services are available for rare conditions like there are for heart attacks and strokes.
However, they also heard about examples of imaginative ways in which local vasculitis ‘champions’ had ‘worked around awkward people and places’ to improve care.
“It is an important platform for raising awareness of vasculitis across all areas of healthcare and highlighting and promoting the increase of positive outcomes from patients attending vasculitis clinics.”
How important are these findings?
We believe this research really matters because:
- The results of this study will now inform guidelines on how best to organise care for people with vasculitis. However, it may take a while for these guidelines to be put into practice.
- It’s influencing policy on how to organise care for people with rare autoimmune rheumatic conditions, such as vasculitis.
- It gave people with vasculitis a voice to talk about their healthcare experiences.
- By hearing other people’s stories, it might make people living with vasculitis feel less alone.
- It’s a fantastic example of how to include patients and the public in research.
“We’re all familiar with clinical trial research to find out what drug treatments, at what doses, are most effective and safe,” says Avril Nicoll, Research Fellow.
“But VOICES demonstrates that the way health services are organised also makes a difference... This is prompting services to think about their patients’ experiences and outcomes and what practical things they can do to improve them.”
Learn more about our research achievementsWhat is next?
Next, the team will explore whether these suggestions could be helpful to health care services looking after people with other rare autoimmune rheumatic conditions, such as: