What is fibromyalgia?
Fibromyalgia is a long-term condition that causes pain and tenderness all over your body.
Unlike arthritis, this isn’t because you have problems with your joints, bones or muscles. It’s thought to be caused by your nervous system in your brain and spine not being able to control or process pain signals from other parts of your body.
The condition is also linked to:
- poor sleep
- feeling you can’t concentrate or remember things
- extreme and constant tiredness that doesn’t improve with sleep or rest – which is known as fatigue.
There can be many other symptoms that affect different parts of your body.
Symptoms
The main symptoms of fibromyalgia are:
- pain – you may feel as though you’ve got pain that spreads throughout your entire body, with certain parts – such as your neck and back – feeling particularly painful
- tiredness, fatigue and generally feeling like you have no energy
- sleeping badly – waking up feeling unrested
- aching and stiffness, which often feels worse during or after you’ve been active.
It’s common for your condition to flare-up, making your symptoms suddenly worse.
Fibromyalgia can also cause:
- forgetfulness or poor concentration
- stress, worry or low mood
- tingling, numbness or swelling of your hands and feet
- headaches
- restless legs syndrome – a tingling, uncomfortable feeling in your legs, especially at night
- irritability, or feeling low or weepy
- feeling like you urgently need to wee, especially at night
- painful menstrual periods
- diarrhoea, constipation and stomach pain – sometimes separately diagnosed as irritable bowel syndrome (IBS)
- increased sensitivity to things like cold, sound, knocks and bumps
- tender or overly sensitive joints and muscles.
The pain may feel like it’s affecting your whole body, or it may be particularly bad in just a few areas. Some people say their pain gets worse in extreme temperatures, such as very hot, cold or damp weather.
People often say that besides the pain, fatigue is the worst part of fibromyalgia. This can be linked to a difficulty to think clearly or remember things properly, which is sometimes called fibro fog or brain fog.
Who gets fibromyalgia?
It’s estimated that somewhere between 1.8 million and 2.9 million people in the UK have fibromyalgia.
It most commonly develops between the ages of 25 and 55, although children can also get it. It appears that more women are diagnosed with fibromyalgia than men.
Does it run in families?
We don’t know for sure whether fibromyalgia can run in families.
It’s thought that people can inherit genes that make them more likely to get fibromyalgia, and the condition can then be triggered by an injury, physical or psychological trauma, or stress.
Causes
We don’t currently know the exact reason why people get fibromyalgia. But there does seem to be a common link with things such as arthritis, a traumatic event, and mental health and well-being.
Fibromyalgia isn’t caused by damage or an injury to the body. But it does increase the sensitivity of your nerve endings, which means you could feel pain from a small amount of pressure or minor knocks.
One theory is that the condition is caused by problems with a person’s central nervous system – which controls all the sensations and movements the body makes.
Studies have shown that parts of the brain that register pain react differently if you have fibromyalgia. This means you feel pain when other people just feel uncomfortable or stiff.
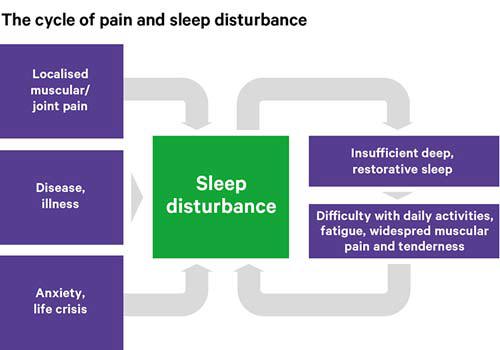
People with fibromyalgia often don’t get enough deep sleep. Research shows that lack of good quality sleep can make pain worse, and maybe even cause pain.
Pain, unhappiness, depression and stress can all make you sleep badly.
Symptoms often start after an illness, accident, or a time of emotional stress and anxiety.
When you’re low or depressed, your pain can also feel worse. At the same time, your pain can make you feel more stressed.
Unlike conditions, such as arthritis, the pain you feel with fibromyalgia isn’t caused by visible inflammation or damage to your body.
This doesn’t mean the symptoms of fibromyalgia are unreal or ‘all in your mind’. However, anxiety, physical or mental trauma, and sleep disturbance are all thought to play a part in the condition.
Diagnosis
Fibromyalgia can sometimes be difficult to diagnose, as the symptoms vary from person to person.
There are some common symptoms your doctor will look for to help diagnose fibromyalgia, including:
- severe pain that has lasted three months or more
- fatigue
- regularly waking up feeling unrefreshed
- problems with your memory and understanding.
It may help your doctor understand the problems you’re having if you make a list of any physical or psychological problems you’ve experienced. They will probably then carry out a physical examination.
There aren’t any specific blood tests, x-rays or scans to confirm a diagnosis of fibromyalgia. But you might have blood tests to check for other conditions.
Many symptoms of fibromyalgia are similar to those of other conditions, such as rheumatoid arthritis, Sjögren’s syndrome (sher-grenz sin-drome) and an underactive thyroid gland.
Some people may be diagnosed and treated for one of these other conditions. It is also possible to have one of these conditions as well as fibromyalgia.
Your doctor may also suggest a referral to:
- a rheumatologist – a doctor who specialises in conditions affecting the bones, joints and muscles. They may confirm your diagnosis.
- a physiotherapist – who can suggest exercises and relaxation techniques
- a clinical psychologist or counsellor – who may use methods such as cognitive behavioural therapy (CBT) and mindfulness
- an occupational therapist – who can advise you on the best way to carry out daily activities and work around your condition
- a community or hospital-based specialist pain clinic, or chronic fatigue service – who can help you manage your symptoms.
What does the future hold for me?
Because fibromyalgia’s symptoms vary from person to person, it’s difficult to predict how long you will have the condition and the impact it will have on your life.
Although there’s currently no cure, there are treatments, therapies and self-management techniques that can improve your quality of life.
Fibromyalgia doesn’t seem to cause long-term damage to your body. But it’s important to keep your muscles and joints strong through activity.
Gradually increasing how much exercise you do can also improve your symptoms.
Treatments
There are a number of ways your symptoms can be managed.
In many cases, fibromyalgia can be diagnosed and treated by your GP, without the need to see a specialist.
They can advise you on treatments and therapies that tackle specific symptoms. These may include drug treatments. However, physical and psychological therapies can often be a more effective way of managing fibromyalgia than medication.
There are also many things you can do for yourself that can change the way your condition impacts upon your life.
Physical therapies
Depending on how your fibromyalgia is affecting you, your doctor may refer you to a physiotherapist or occupational therapist.
Physiotherapy
Physiotherapy can help relieve the pain of fibromyalgia.
Physiotherapists are trained specialists who can help you stay active and independent. They will show you the best exercises to strengthen your muscles, without hurting yourself or putting your body under too much strain.
They can show you how something as simple as improving your posture can help your pain. They may also advise you on relaxation techniques which can be just as important as exercise when you’re dealing with fibromyalgia.
Your doctor can refer you to an NHS physiotherapist. In some areas you can refer yourself, but this may take a while.
It can be quicker to see a physiotherapist privately, but you would pay for the appointment. To find a private physiotherapist, visit the Chartered Society of Physiotherapy website.
Occupational therapy
Occupational therapy can help you manage your everyday activities around your fibromyalgia, without increasing your pain or overwhelming yourself.
Your occupational therapist may suggest new ways you can get things done. They may also teach you some relaxation techniques.
If you still find some activities difficult after you’ve made these changes, they may suggest equipment, known as aids and adaptations, to help you.
Your doctor can refer you to an occupational therapist or you can see one privately, for a fee.
To find a private occupational therapist, visit the Royal College of Occupational Therapists website.
If you’re having problems at work, your employer may have an occupational health team that could help you. Otherwise, you can contact a Jobcentre Plus office to ask for advice.
Acupuncture
Your doctor may recommend a course of acupuncture from a trained NHS healthcare professional, such as a physiotherapist, to help with your pain. You may be able to receive this treatment at a local health centre or GP surgery.
Acupuncture uses fine needles, inserted into several specific parts of the body to relieve pain. There is evidence to support its use in the short-term treatment of fibromyalgia. Though a course of treatments may only help for up to three months, it may help you start managing your condition.
Doctors will not recommend treatment with devices such as TENS machines, ultrasound or interferential therapy, because there is currently little evidence to support their use in treating fibromyalgia.
Pain clinics and pain management programmes
Pain clinics bring together the skills of a wide range of professionals, such as:
- specialist pain consultants
- physiotherapists
- occupational therapists
- psychologists
- social workers
- employment advisors.
They can provide specific treatments or rehabilitation therapies that could reduce the effects of fibromyalgia.
A pain specialist may suggest you join a pain management programme, which brings together people with different long-term pain conditions. Pain management won’t take away your pain, but it can help you manage it better and reduce its impact on your life.
These sessions are often led by psychologists who specialise in helping people find ways to live with their pain. They are usually held in an outpatient clinic and run over several days or weeks.
Psychological therapies
Pain is never just a physical experience, especially if it lasts a long time. Pain can affect your mood and behaviour.
Psychological approaches to pain management try to address the emotional effects of your pain and the things that can make your pain worse. They help you look at how your pain affects your thoughts and habits, and how your emotions can affect your pain.
Therapies such as cognitive behavioural therapy (CBT), which is a talking therapy, try to reduce the overwhelming effect of problems such as stress, unhappiness and pain.
They aim to help you understand how you react to different problems by breaking them down into smaller, more manageable, chunks. This should help you change the way you react to them and the effect they have on you.
Making small changes to the way you react to a situation or problem can often improve both your emotional and physical health.
Psychological therapies can also include relaxation techniques and other ways to reduce your stress.
They encourage you not to be too hard on yourself, even when you feel frustrated, and to accept that sometimes there are limits to what you can do.
A number of healthcare professionals often have training in CBT, so you may not have to see a psychologist.
For more information about psychological therapies and CBT, the British Association for Behavioural & Cognitive Psychotherapies (BABCP) keeps a register of all accredited therapists in the UK.
Drug treatments
Drugs can’t treat fibromyalgia, but they can help reduce your symptoms. Your doctor may only recommend drug treatment once you've tried options such as exercise, psychological therapy or acupuncture.
Before prescribing drugs to treat your pain, your doctor will discuss the benefits and risks of starting drug treatment. If you are aged over 18, it’s likely they will first try you on an antidepressant, such as:
- amitriptyline
- citalopram
- duloxetine
- fluoexetine
- paroxetine
- sertraline.
Antidepressants are regularly used to treat sleep problems and pain, as well as depression. When they are used to treat pain, they’re usually prescribed at a lower dose than when they are used to treat depression. However, they can still help if your condition effects your mood.
Antidepressants are now recommended by the National Institute of Health and Care Excellence (NICE) as the first choice of drug treatment for unexplained long-term, widespread pain, such as fibromyalgia.
You might need to take them for a few months before you feel their full benefits. Your doctor will gradually increase the dose to a level that works for you.
Some antidepressants can make you feel sleepy, so avoid taking them before you drive, cycle or use heavy machinery. You usually need to take them about two hours before bedtime.
All drugs have potential side effects. It’s important to talk to your doctor about how to get the best balance between pain relief and any unpleasant effects. If you feel like a treatment isn’t helping you, talk to your doctor.
In the past people with fibromyalgia have been prescribed a variety of different types of drugs, such as:
- gabapentin and pregabalin, which target nerve pain
- opioid painkillers, such as codeine, tramadol, and morphine
- compound painkillers, including co-codamol and co-dydramol
- paracetamol
- non-steroidal anti-inflammatory (NSAIDs), such as ibuprofen and naproxen
- steroid injections.
If you are currently prescribed one of these drugs, your doctor is likely to want to discuss whether your condition could be treated differently in the future.
How can I help myself?
Exercise
If you’re in pain, your instinct may be to avoid exercise or moving around too much. But keeping active is a really important part of the treatment for fibromyalgia and can prevent other health problems.
Your symptoms and general health can be improved by a combination of aerobic exercise and movements that improve your flexibility and strength.
Exercise has been proven to improve fatigue and our ability to control pain.
At first, you may find that your pain and tiredness become worse, particularly if you’re starting to exercise muscles that haven’t been used for a while. Try to do the same amount of exercise each day, so you build up your muscle strength and your stamina.
Then, after doing your routine of exercises for a couple of weeks, slowly increase the amount you do, and this will improve your fitness, stamina and flexibility.
Aerobic exercises
Aerobic exercise is anything that makes you a little out of breath and your heart beat faster.
Swimming is recommended for people with fibromyalgia. Taking a brisk walk and cycling can also help.
At home, you could step up and down your bottom step several times, or march on the spot to get your heart beating faster.
Strengthening exercises
Strengthening exercises help develop and build the muscles that move and protect your joints. They may be difficult at first but should become easier with practice.
Aim to do at least one session a day, either at home or in a gym. Ask a GP or physiotherapist for examples of strengthening exercises you could do at home.
You can also buy specially designed equipment, such as ankle weights. Begin with lighter weights, then move on to heavier ones, if you feel able to.
Strengthening equipment in a gym allows you to work your muscles by pushing or pulling against a resistance, such as weights or elastic ropes. You can ask an instructor for advice about using the equipment, if you’re not sure.
Stretching exercises
Stretching, or range of movement, exercises can increase your flexibility. You can do these anywhere. There are plenty of examples of exercises online, or you could ask a physiotherapist. Some people with fibromyalgia have found Tai chi and yoga help.
Diet and nutrition
There’s no particular diet that’s been proven to help fibromyalgia. However, it’s recommended that you keep to a healthy weight by eating a balanced diet that is low in saturated fats, sugar and salt, and has plenty of fruit and vegetables. It’s also good to drink six to eight glasses of water every day.
Complementary treatments
Some people with fibromyalgia find that complementary treatments help their symptoms.
Massage can also be helpful for some people with fibromyalgia. However, the effects don’t often last that long.
If you want to try a complementary treatment, speak to your doctor first, in case it affects any other treatment you’re on.
It’s important to go to a legally registered therapist, or one who has a set ethical code and is fully insured.
If you decide to try therapies or supplements, you should be critical of what they’re doing for you and only continue if they’re helping.
Sleep
Poor sleep appears to be a significant cause of fibromyalgia, so getting enough good-quality sleep is an important part of your treatment. Not only will it help with tiredness and fatigue, it may also improve your pain.
Sleeping tablets are not normally recommended, as the body can become tolerant to them, which can lead to the effects wearing off and even addiction. But regular activity, particularly aerobic exercise, and cognitive behavioural therapy (CBT) have proven effective for people with disrupted sleep patterns.
It can also help to change your habits around bedtime. To help you get a better night’s sleep:
- Make sure your bedroom is dark, quiet and a comfortable temperature.
- Try a warm bath before bedtime to help ease pain and stiffness.
- Develop a regular routine, where you go to bed and get up at a similar time each day.
- You may like to try listening to some soothing music before going to bed.
- Some gentle exercises may help reduce muscle tension, but it’s probably best to avoid energetic exercise too close to bedtime.
- Keep a notepad by your bed – if you think of something you need to do the next day, write it down and then put it out of your mind.
- Avoid caffeine in the eight hours before you go to bed.
- Don’t drink alcohol close to bedtime.
- Avoid eating main meals close to bedtime.
- If you smoke, try to stop smoking, or at least don’t smoke close to bedtime.
- Try not to sleep during the day.
- Avoid watching TV and using computers, tablets or smartphones in your bedroom.
- Don’t keep checking the time during the night.
What else can I do?
Because fibromyalgia varies from person to person, we suggest you try some of the following tips to find out what works for you:
- Learn about fibromyalgia – understanding your condition can help reduce your fears and anxiety. It also means you’re fully aware of treatment and self-management approaches that can help you.
- Find a support group in your area or an online forum for people with fibromyalgia. Talking about your experiences with other people who understand can help.
- Encourage your family and friends to learn more about your condition and to talk to you about it. You could show them this information. It’s especially important they understand how your pain affects you, even if you look well.
- Find ways to talk about your feelings, such as anxiety, low mood or anger. Counselling or CBT can help – your GP will be able to refer you.
- For ‘fibro fog’, some people find mental exercises like crosswords or jigsaw puzzles help. Do as much as you can to stimulate your brain.
- Pick your best time of day to do anything needing concentration. Explain to others if fibromyalgia affects your memory.
- Learn to pace yourself by breaking tasks into smaller chunks, giving yourself time to rest in between.
- Stress and unhappiness can make fibromyalgia pain feel worse – addressing what’s making you feel that way could help.
- Ask for help from people at your workplace, such as a friend, colleague or manager.
- Working shorter hours, as well as adapting your desk, chair, computer and other working areas for comfort, can all help.
- Ask an occupational therapist, your local Jobcentre Plus office or Citizens Advice service for advice. They can work with both you and your employer.
- Applying heat with a hot water bottle, or having a hot bath or shower, can help pain and improve morning stiffness.
- If you have a dry mouth, try a toothpaste containing sodium bicarbonate.
- Some people have found meditation helps improve their pain.
- Try the treatments your doctor offers and discuss which ones are helpful.
Research and new developments
Versus Arthritis is funding a number of research studies into the causes, effects and treatment of fibromyalgia. Some examples include:
- A study at the University of Cambridge is looking at why things that wouldn’t normally be painful, such as sound, light and gentle touch become painful for people with fibromyalgia, and whether brain signals that process pain differ in people with fibromyalgia.
- Research underway at the University of Sussex is examining how the bodies’ natural fight and flight response to stress might be altered in people who have fibromyalgia. This work is also looking at the role inflammation might have in this process.
- We are funding work at the University of Liverpool investigating how the brain processes pain signals. It has been found that in people with long-term pain such as fibromyalgia there are differences in the structure and activity in the parts of the brain that process pain signals. Using mathematical modelling, this work could help to match people up with the best treatment option for them.
- We are also investigating how to improve healthcare services for people with fibromyalgia. Research being carried out at the University of Aberdeen is looking at how long it took people with fibromyalgia to get diagnosed and where in the system improvements can be made.
The Pain Centre Versus Arthritis
In partnership with the University of Nottingham and local NHS Trusts, Versus Arthritis supports the world’s first national centre for research into pain.
The aims of the centre are to improve our understanding of pain and ways to stop it, through existing and new treatments.
The centre has experts in rheumatology, neuroimaging, psychology, neuropharmacology, neurosciences and orthopaedic surgery.
Lynn's story
 Lynn White was diagnosed with fibromyalgia in her early 40s. Now at 52, she wants people to know they can keep on top of their condition with treatment, self-care and the occasional treat.
Lynn White was diagnosed with fibromyalgia in her early 40s. Now at 52, she wants people to know they can keep on top of their condition with treatment, self-care and the occasional treat.
‘I had the symptoms for years before I found out I had fibro. I knew I wasn’t right. I’d feel awful.
‘I’d get terribly low and I was in pain everywhere. But you just get on with things don’t you. I didn’t want to make an issue out of it. My daughter has JIA and Sjogren’s syndrome and she was so ill, I couldn’t think about how I was feeling.
‘When I eventually saw a rheumatologist, she just pressed my trigger points - I went through the roof. Tears were pouring down my face.
‘Knowing I had fibro made such a difference. When you can name it, you can start dealing with it.
‘I have to look after myself. I try to pace myself. I exercise with a personal trainer too, that makes all the difference.
‘Exercise is so important. But don’t just go and exercise, you need to see a physiotherapist or a gym instructor. Doing the wrong exercises can be as harmful as doing nothing. Make yourself keep walking, because when you stop it’s so difficult to get going again.
‘I have acupuncture, laser and heat treatments. They’re brilliant and really help. If I don’t go it takes weeks to get back on track.
‘I get as much sleep as I can. In the morning I’m still tired and my legs feel like lead, but I must get on and walk the dogs. Heat pads on my waist really help me walk. I always feel much better out in the fresh air.
‘I watch my diet, because once the weight goes on it doesn’t shift, that makes me feel worse.
‘If I’m going out, I try not to do too much the day before and after. Sometimes, I really don’t feel up to it, but my friends really understand.
‘I have down days, but I deal with it. It helps to stay positive. It would be very easy to get down.
‘I make sure I treat myself with a massage or a facial. It’s not indulgent, it helps. It’s so important to relax your body, mind and muscles and I know I’ll sleep well that night.
‘Little things really do make a difference. I still have days I don’t feel great, but I know I have to get on with things.’