What is osteoarthritis of the knee?
Osteoarthritis (os-tee-o-arth-ri-tus) is the most common form of arthritis, and the knee is one of the most commonly affected joints.
Everyone’s joints go through a normal cycle of damage and repair during their lifetime, but sometimes the body’s process to repair our joints can cause changes in their shape or structure. When these changes happen in one or more of your joints, it’s known as osteoarthritis.
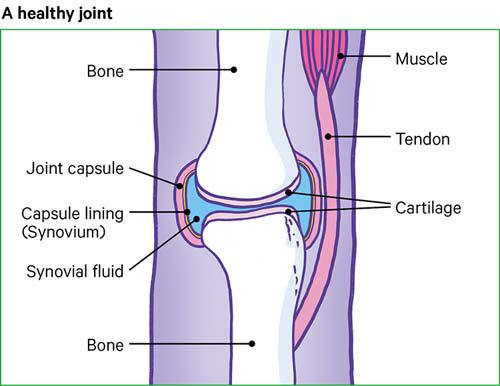
A joint is a part of the body where two or more bones meet – in your knee, it’s the thigh and shin bones. There is also a small bone at the front of the knee called the patella or kneecap.
The ends of our bones are covered in a smooth and slippery surface, known as cartilage (car-ti-lidge). This allows the bones to move against each other without friction, and protects your joint from stress.
Your knee also has two other rings of a different type of cartilage known as menisci or meniscus, which help to share weight evenly across your knee joint, and there’s also cartilage underneath your kneecap.
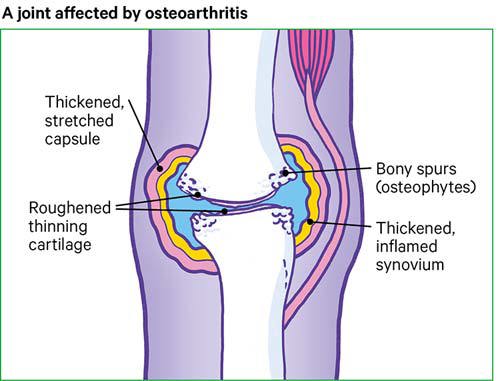
Osteoarthritis causes the cartilage in your knee joint to thin and the surfaces of the joint to become rougher, which means that the knee doesn’t move as smoothly as it should, and it might feel painful and stiff.
Osteoarthritis can affect anyone at any age, but it’s more common in women over 50.
Injuries or other joint problems, such as gout, can make people more likely to get osteoarthritis. The genes we inherit from our parents can also increase the risk of the condition developing.
Being overweight is also linked to osteoarthritis, as this causes extra strain on weight-bearing joints, such as your knees.
How will it affect me?
If you have osteoarthritis of the knee, you will probably feel your knee is painful and stiff at times. It may only affect one knee, especially if you’ve injured it in the past, or you could have it in both. The pain may feel worse at the end of the day, or when you move your knee, and it may improve when you rest. You might have some stiffness in the morning, but this won’t usually last more than half an hour.
The pain can be felt all around your knee, or just in a certain place such as the front and sides. It might feel worse after moving your knee in a particular way, such as going up or down stairs.
Sometimes, people have pain that wakes them up in the night. You’ll probably find that the pain varies and that you have good and bad days.
You might find you can’t move your knee as easily or as far as normal, or it might creak or crunch as you move it.
Sometimes your knee might look swollen. This can be caused by two things:
- Hard swelling: when the bone at the edge of the joint grows outwards, forming bony spurs, called osteophytes (os-tee-o-fites).
- Soft swelling: when your joint becomes inflamed and produces extra fluid, sometimes called an effusion or water on the knee.
Sometimes osteoarthritis of the knee can cause the muscles in the thighs to weaken, so your leg may look thinner. This weakness can make the joint feel unstable and could cause the knee to give way when you put weight on it.
The effects of osteoarthritis can make people feel depressed or anxious, and it can affect relationships and sleep. If you have any problems like this, mention them to your doctor as there are things they can do to help.
Are there any complications?
Osteoarthritis can develop over just a year or two, but more often it’s a slow process over many years that only causes fairly small changes in just part of the knee.
But in some cases, the cartilage can become so thin that it no longer covers the ends of the bones. This causes them to rub against each other and eventually wear away.
The loss of cartilage, the wearing of the bones, and the bony spurs can change the shape of the joint. This forces the bones out of their normal positions, making your knee feel unstable and painful.
Some people with osteoarthritis find a lump appears at the back of their knee. This is called a Baker’s cyst or popliteal cyst.
A Baker’s cyst is fluid-filled swelling at the back of the knee that happens when part of the joint lining bulges through a small tear in the joint capsule. This can then cause joint fluid to be trapped in the bulge.
It can happen on its own, but is more likely in a knee that’s already affected by arthritis. A Baker’s cyst doesn’t always cause pain, but sometimes they can burst so the fluid leaks down into your calf, causing sharp pain, swelling and redness in the calf.
Osteoarthritis in the knee might change the way you walk or carry your weight, and this could cause you to develop the condition in other joints, such as your hips.
Managing osteoarthritis of the knee
There’s no cure for osteoarthritis, but there are things you can do for yourself that can make a difference to how the condition affects you. There are also some treatments available that could significantly reduce your pain.
Exercise
Joints need to be exercised regularly to keep them healthy. It’s very important to keep moving if you have osteoarthritis of the knee. Whatever your fitness level, exercise helps the knee to be able to cope with normal daily activities again.
You’ll need to find the right balance between rest and exercise – most people with osteoarthritis find that too much activity increases their pain while too little makes their joints stiffen up. Exercise can strengthen the muscles around your knee, improve your posture and help you to lose weight, all of which can reduce the symptoms and pain of osteoarthritis.
It’s important to carry on with your exercises even if you start to feel better, as stopping or reducing the amount of exercise you do could cause your symptoms to come back again. A physiotherapist can advise you on the best exercises to do, but you’ll need to build them into your daily routine to get the most benefit from them.
Your physiotherapist may recommend exercise in a hydrotherapy pool. This can help get muscles and joints working better and, because the water is warmer than in a normal swimming pool, it can be very soothing and relaxing. Hydrotherapy is sometimes called aquatic therapy.
Swimming and exercising in water can be helpful if your joints are painful, as the water takes the weight of your body which reduces any strain on your knees, but still lets you keep moving. It’s important to balance this with weight-bearing exercise as well, such as walking, as this will help to keep your bones strong.
There are various types of exercise that have been proven to help treat osteoarthritis of the knee. You can try some examples on our exercises for the knees page.
Range of movement exercises
These are good for posture and helping to keep your joints flexible. These exercises can be something as simple as stretching, making sure your joint moves through a range of positions that comfortably stretch its reach and flexibility slightly further each time.
Strengthening exercises
This type of exercise is important to improve the strength of the muscles that control your knee, and to help stabilise and protect the joint. It’s also been shown to reduce pain and can prevent your knee giving way, reducing the risk of falls.
You should try to do strengthening exercises on at least two days a week if you can.
Aerobic exercise
Aerobic exercise is any exercise that increases your pulse rate and makes you a bit short of breath. Regular aerobic exercise can help you in many ways. It’s good for your general health and well-being and can reduce pain by stimulating the release of pain-relieving hormones called endorphins. It can also help you sleep better.
Different types of aerobic exercise include cycling, swimming and walking. You should work hard enough to get out of breath but still be able to have a conversation.
You should try to do 2 hours and 30 minutes of aerobic exercise each week. You can spread this out over the week and don’t need to do it all in one go.
Weight management
Being overweight increases the strain on your joints, especially your knees. It makes it more likely that you’ll develop osteoarthritis and that your arthritis will get worse over time.
Losing weight if you’re overweight could reduce your pain and other symptoms of osteoarthritis of the knee. The force put through your knees when you walk, run or go up and down stairs can be two or three times your body weight, so losing even a small amount of weight can make a big difference to the strain on your knees.
There’s no special diet that will help with osteoarthritis, but if you need to lose some weight you should follow a balanced, reduced-calorie diet combined with regular exercise. Your doctor should be able to give you advice on diets and exercise that will help.
Reducing the strain on your knees
Apart from keeping an eye on your weight, there are a number of other ways you can reduce the strain on your knees.
- Pace your activities – don’t tackle all your physical jobs at once. Break the harder jobs up into chunks and do something gentler in between. Keep using your knee even if it’s slightly uncomfortable, but rest it before it becomes too painful.
- Wear shoes with thick soles and enough room for your toes. Wearing the right shoes can reduce the shock through your knees as you walk and prevent any changes to your feet.
- If you need extra support for your feet or knees when you walk, speak to your physiotherapist, occupational therapist or doctor about getting insoles made for your shoes.
- Use a walking stick if needed to reduce the weight and stress on a painful knee. An occupational therapist can advise on the correct length and the best way to use the stick.
- Use a handrail for support when going up or down stairs. Go upstairs one at a time with your good leg first.
- Think about making changes to your home, car or workplace to reduce unnecessary strain. An occupational therapist can advise you on special equipment that will make things you do every day easier.
Using a heat pack or something similar on a painful knee might help to relieve the pain and stiffness of osteoarthritis. An ice pack can also help but be careful not to put ice or heat packs or hot water bottles directly on your skin – wrap them with a tea towel or cover.
Some people find that knee braces help. You can buy knee braces from sports shops and chemists, but you should speak to your doctor or physiotherapist first, as they might be able to provide braces or recommend the best one for you.
Coping with low mood and sleep problems
You might find that osteoarthritis of the knee makes you feel depressed or anxious. Speak to your doctor if you’re feeling low as they may be able to recommend psychological therapies to help you, such as cognitive behavioural therapy (CBT) and stress-relieving techniques.
If your sleep is disturbed because of osteoarthritis of the knee, this could make your pain feel worse. However, there are things you can do for yourself that might help, such as:
- Keep a sleep diary to work out if there are any patterns to your sleep problems
- Sleep at regular times to get your body into a routine
- Avoid phones and other screens in the bedroom to help you wind down before bed.
If you’re still having problems, speak to your doctor or an occupational therapist who can give you other tips and techniques to try, known as sleep hygiene.
Drugs
Drugs can be used to help ease the pain and stiffness caused by osteoarthritis, but they won’t prevent or cure the condition itself. You’ll have the best results if you keep active, reduce the strain on your knees, and take drugs for your condition as you need them.
Some of the drugs and treatments you can try include:
- Painkillers: simple over-the-counter painkillers such as paracetamol may help, but your doctor may prescribe you stronger painkillers if needed.
- Non-steroidal anti-inflammatory drugs (NSAIDs): a short course of NSAIDs, such as ibuprofen, can help reduce any pain, inflammation and swelling in your knee.
- Steroid injections: an injection directly into the knee joint, which can help reduce swelling and pain.
If you’re taking any of the over-the-counter medications mentioned above, make sure you’re taking them safely and as directed by your doctor or the patient information leaflet included with the drug. Make sure whoever is treating you knows all the medications you’re taking,
Other pain relief
If the methods of pain relief above don’t help you, you might want to try some of the following:
- Transcutaneous electrical nerve stimulation (TENS): a small machine that changes the way nerves understand pain by sending tiny electric shocks through pads placed on your skin.
- Hyaluronic acid injections: hyaluronic acid occurs naturally in the body and helps to lubricate joints. These injections aren’t available on the NHS as they’ve not been proven to be effective, but you may be able to get them privately.
- Complementary treatments and supplements: some people with osteoarthritis find glucosamine and chondroitin helpful, but you should talk to your doctor before you start taking anything new, as there isn’t a lot of research to show that these are helpful and they may interact with some prescribed drugs.
Surgery
Exercise, treatments and keeping to a healthy weight usually improve the symptoms, pain and ability to do daily activities in most people with osteoarthritis of the knee. But if these treatments haven’t worked for you, you may benefit from having surgery on your knee.
Surgery might be suggested if your pain is very severe or if you have problems getting around or moving your knee.
The most common type of surgery for osteoarthritis of the knee is a knee replacement. Many knee replacements are performed each year, and the operation can give a lot of pain relief and improve movement in your knee.
Surgical techniques are improving all the time and research has shown that up to 8 in 10 knee replacements could last as long as 25 years. However, as with all surgery, there are some risks and your surgeon will want to make sure you’re in the best health possible before the operation.
Sometimes keyhole surgery techniques may be used to wash out loose fragments of bone and other tissue from your knee. This is called arthroscopic lavage (arth-row-scop-ick lav-arge) or debridement, but it won’t be recommended for you unless your knee locks.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.