How do the feet and ankles work?
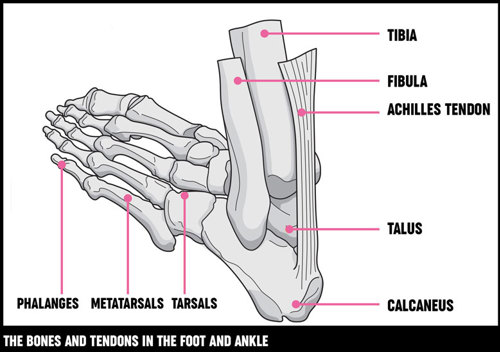
Our feet are made up of 26 bones and more than 33 joints arranged in columns and arches that vary in stiffness and flexibility. Many common problems can occur in this complex structure.
The foot is usually separated into three different parts:
The back of your foot (hindfoot) is made up of your heel bone (calcaneus) and your ankle (talus). They’re joined together by your subtalar joint, which allows your foot to move from side to side.
Your ankle bone is joined to your leg bones (tibia and fibula) at your ankle joint, which acts like a hinge. This allows your foot to bend up and down.
The middle of your foot (midfoot) is made up of five tarsal bones. These form the arch of your foot. Your tarsal bones are connected to the front and back of your foot by muscles and the arch ligament (the plantar fascia). They act as shock absorbers when we’re walking or running.
The front of your foot (forefoot) is made up of your toe bones (phalanges), which are connected to five long bones (metatarsals) by joints. The joints in your toes don’t move very much. Your forefoot takes half of your body’s weight.
The muscles in your lower leg are attached to bones in your feet by tendons, and they control movement that allows us to stand, walk, go on tiptoes and jump. These muscles move your toes and control the position of your foot as it hits the ground, allowing it to become flexible and cushioning the impact. They also make the arches of your feet more rigid to push your body forward when you move.
Your heel bone is connected to the calf muscles in your lower leg by your Achilles tendon, which is the most important tendon for movement. The tibialis posterior tendon, which attaches the underside of your foot to your lower leg, helps supports the arch of your foot and allows you to turn it inward.
The main nerve of your foot controls the muscles in your sole and gives feeling here and to your toes. Other nerves give feeling to the top and outside edge of your foot.
Do I need surgery?
Most people with problems in their feet or ankles won’t need surgery. The decision whether to operate depends on a number of factors:
- how bad your symptoms are (pain and the effect this has on your life)
- your needs
- your response to other treatments, including drugs, orthoses and special footwear.
Discuss these with your healthcare professionals, who’ll be able to advise you on whether they think surgery would be a suitable option.
The decision to have foot and ankle surgery is usually based on lifestyle choices and the information given by surgeons rather than being essential in terms of life and death. But if your skin is affected or your feet are quickly becoming deformed, it’s important to get an assessment for urgent surgery to avoid infection and alert your healthcare professionals to possible stress fractures. You’ll always have the final decision on whether to have the operation.
You may feel nervous, stressed or scared if you’ve been told you need surgery. Finding out as much as you can about the operation and understanding the process will help you feel calmer and more in control.
Common types
Conditions that may need surgery include bunions and hammer toes, ankle arthritis, Achilles tendon disorders and plantar fasciitis.
Bunions
Bunions are bony lumps that develop on the side of your foot and at the base of your big toe. They’re the result of a condition called hallux valgus, which causes your big toe joint to bend towards the other toes and become deformed. If symptoms carry on over a long period, your toe may need to be surgically corrected. This involves straightening your big toe and metatarsals, a process called an osteotomy. Although this may make your joint stiffer, it works to ease the pain.
Most surgery can be performed as a day case and takes up to an hour. Your foot will be bandaged and you’ll need to wear a Velcro surgical shoe for four to six weeks afterwards.
If your bunion has been caused by rheumatoid arthritis, you may also develop rheumatoid nodules. These firm, pea-sized lumps can occur at pressure points such as your big toe joints, the back of your heels or on your toes, but they can be surgically removed.
Sometimes swellings or bursae on the joints in your feet are also called bunions, but these aren’t the same as bunions caused by hallux valgus and don’t need surgery.
Hallux valgus is different to hallux rigidus, which is osteoarthritis of the big toe joint. Hallux rigidus causes stiffness in your big toe and you won’t be able to move it as far. If treated early, surgery can be used to remove painful osteophytes (overgrowth of new bone) that can develop and allow more joint movement to return. In more advanced cases, fusion surgery (joining bones together to make one stiff bone where there two) gives excellent pain relief, although it will mean that the joint will no longer bend when you walk so you won’t be able to wear high-heeled shoes.
Hammer toes
As well as bunions, hallux valgus can also cause your other toes to become clawed or permanently bent. This condition is known as hammer toes. Damages caused by hammer toes can be eased by:
- arthroplasty – removing the deformed joint between your toe bones (phalanges), which leaves the joint flexible
- arthrodesis – fusing your phalanges together, which leaves your toe more stable but means you’ll only be able to wear flat shoes after the operation.
Both procedures are performed as day cases and last around an hour. Your stitches will be removed about two to three weeks following surgery and you’ll need another dressing for two to six weeks after that. You should limit how much you walk for the first three days.
Metatarsal
The joints in your forefoot can be damaged by inflammation of the lining of your joint (synovitis) in some forms of arthritis, for example rheumatoid arthritis. These small joints are called the metatarsophalangeal joints (MTPJs), and they can become dislocated when damaged by arthritis. The pain and discomfort this causes is sometimes described as feeling like you’re walking on pebbles.
If your symptoms are severe and can’t be controlled by other treatment, you may need surgery. The exact surgical procedure and the follow-up you’ll need will depend on how severe the problem is, but often surgery to your big toe and removal of the heads of your MTPJs is carried out in order to make your foot more comfortable and walking easier. Your surgeon will be able to give you more information before the operation.
Ankle arthritis
Ankle arthritis is usually caused by osteoarthritis. This is where the cartilage covering the ends of your bones gradually roughens and becomes thin, and the bone underneath thickens.
It can also be caused by damage from other rheumatic conditions, for example if you have rheumatoid arthritis, or if you’ve had a previous injury to the area. This leads to pain, swelling and occasional deformity of the joint. You may need surgery if your symptoms are severe. There are three surgical options:
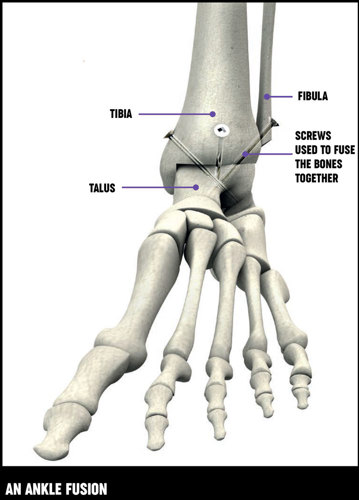
Ankle fusion – Ankle fusion involves removing the damaged ankle joint and fusing your talus bone to your tibia to form a stiff but pain-free ankle. Your foot is fused at a right angle to your leg, in the position it would be if you were standing up. Your bones are held together using screws and new bone grows across, creating one bone where there were two. It normally takes between 12–14 weeks for the fusion to be complete and your bone continues to become stronger after this.
In some cases this procedure can be performed using keyhole surgery (arthroscopy), which means it can be done through just a small cut, so your joint doesn’t have to be opened up. The procedure takes between one and two hours.
After surgery you’ll need to wear a cast for 6–12 weeks, depending on your situation. You should be able to wear normal shoes after the cast is removed, although some alterations are occasionally needed. It should be easier to walk normally or even more comfortably than you did before surgery if your other joints aren’t affected by arthritis, but running isn’t recommended.
Triple fusion – Triple fusion is the surgical fusion of three joints (the talonavicular, subtalar and calcaneocuboid joints) either as a treatment for arthritis within these joints or as a method of correcting a stiff foot deformity. A combination of plates, screws or staples is often used to do this. It takes 12–14 weeks for the fusion to be complete.
Ankle replacement – An ankle replacement involves taking out the worn-out ends of your tibia and talus bones and replacing them with a man-made (artificial) ends made out of plastic or metal. Unlike an ankle fusion, a replacement allows you to move your joint after surgery.
The procedure takes between one and two hours and you’ll normally need to stay in hospital for two days. Your foot will be put in a temporary cast afterwards but then it’ll be bandaged and you may need a splint for support. This allows you to move it fairly soon after surgery, but you’ll probably need to use crutches for about six weeks.
Replacement ankle joints haven’t been used for as long as replacement hips and knees, and they don’t last as long, but they can last for about 10–15 years. Your occupational therapist or physiotherapist will advise you on how to take care of the new joint.
As with all joint replacements, there’s a chance that your new joint will wear away over time and you may need to have it removed to have ankle fusion surgery. Fusion after a replacement is harder to do than a primary fusion and more bone may need to be removed. You may need a bone graft (where bone is taken from elsewhere in your body, normally your pelvis) to replace the removed bone. This is quite a common procedure, and ankle fusion following a replacement is usually very successful.
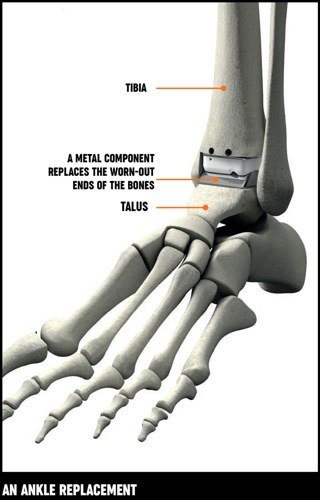
Versus Arthritis have recently awarded a grant for the OARS study, which will assess the major factors that predict what patients think (patient-reported outcome) in the first year after total ankle replacement.
Achilles tendon disorders
Your Achilles tendon is the largest tendon in your body, and the muscle in your lower leg puts a lot of force through it to make you move. As we get older it can start to wear, which can lead to painful swellings within the main tendon or where it attaches to your heel bone. Very occasionally surgery can be used as a method of treatment. This procedure is usually performed as a day case and you’ll need to wear a bandage and use crutches afterwards.
Morton’s neuroma
Morton’s neuroma is a painful condition that involves a nerve that supplies feeling to two neighbouring toes. It most commonly affects the nerve to your third and fourth toes. If your symptoms are bad, surgery to remove the painful nerve can be successful. This can be done as a day case and you’ll need to wear a bandage for two weeks afterwards.
Tibialis posterior disorder
The tibialis posterior is a muscle that supports the shape of your instep arch. The tendon that connects this muscle to the bone can become inflamed, leading to pain and swelling on the inside of your ankle. Continual swelling can start to cause the tendon to weaken, which can lead to a flatfooted look.
Occasionally, bad cases need surgery to rebuild the instep arch. If your case is long-standing or you haven’t had treatment, three of your hindfoot joints may need to be fused (triple fusion) to ease pain.
Both operations take between one and two hours and you’ll need to wear a plaster cast for 6–12 weeks after.
Plantar fasciitis
The plantar fascia is a tough band of fibrous tissue that starts at your heel bone and stretches across the sole of your foot to your toes. Plantar fasciitis is inflammation at the site where the fascia attaches under your heel. Very rarely, bad cases may need surgery to release the plantar fascia from the heel bone.
This procedure is usually performed as a day case and it takes less than an hour. You’ll only need to wear a bandage after the operation.
Advantages
The main advantages of foot and ankle surgery are:
- long-lasting pain relief
- better function and mobility
- a greater choice of comfortable footwear improved appearance of your feet, depending on the procedure.
Disadvantages
As with any surgery, results can vary from person to person and there can occasionally be complications.
There are some possible disadvantages to foot and ankle surgery:
- Replacement joints aren’t as hard-wearing or long-lasting as natural joints.
- Some operations restrict joint movement (although this doesn’t mean that it’ll reduce your mobility).
- You may not be able to use your foot properly for some time after the operation (for example, you may need to keep weight off your foot for three months after an ankle fusion). This can be a particular problem if you’re likely to have problems getting around using crutches.
- Occasionally small nerves around the cut in your skin (the incision) can be damaged, leading to patches of numbness.
- There can be complications during surgery, for example swelling, stiffness or infection.
- In some cases where bones are joined (fused) together, the bones can take longer to fuse together than expected and you won’t be able to use your foot properly during this time. Occasionally a non-union occurs – where the fusion doesn’t work properly – and you may need further surgery.
Alternatives
Alternatives to foot and ankle surgery may include exercise, footcare, drug treatment and specially modified shoes.
Most people with foot and ankle problems will receive other treatments from their GP, rheumatologist or podiatrist before they see a surgeon for an operation. These may include:
- exercise
- footcare
- drug treatments, usually painkillers and non-steroidal anti-inflammatory drugs (NSAIDs)
- disease-modifying anti-rheumatic drugs (DMARDs) if you have rheumatoid arthritis
- steroid injections
- advice on footwear style
- insoles/orthoses and specially altered shoes.
If these treatments don’t ease the pain then your doctor may suggest you have surgery.
Complications
Complications of foot and ankle surgery can include infections, swelling and stiffness, and wound haematoma (bleeding).
If you’re generally healthy the risk of a serious complication from an operation is very small. Every possible care is taken to prevent complications, but in a few cases these do happen. For example, some people can develop an infection, so it’s important to speak to your doctor straight away for antibiotic treatment if you notice any signs, including:
- increased pain
- redness
- the affected area feeling warmer than usual
- an unpleasant smell
Some people may have swelling and stiffness, but physiotherapists and occupational therapists can help with exercises and other advice.
Bleeding and wound haematoma
A wound haematoma is when blood collects in a wound. It’s normal to have a small amount of blood leak from the wound after any surgery, and usually this stops within a couple of days. But occasionally blood may collect under your skin, causing a swelling. This can cause a larger but temporary leakage from the wound usually a week or so after surgery, or it may require a smaller second operation to remove the blood collection. Drugs like aspirin and antibiotics can increase the risk of haematoma after surgery.
Preparing for surgery
Before your surgery, your doctor or nurse will check your general health and give you information about preparing for surgery. Ask about any possible changes to your medication and any other questions you may have.
Before the operation your doctor will discuss how long you’ll need to stay and what you’ll need to do before surgery with you. This may include not eating or drinking for a few hours before your operation.
You’ll be asked to sign a consent form that gives your surgeon permission to carry out the treatment. It’s important to ask any questions you may still have. Ask your doctor, nurse or therapist to explain anything you don’t understand. This will help if you’re feeling a little worried.
You should also discuss with your surgeon, anaesthetist or nurse whether you should stop taking any of your medications or make any changes to the dosage or timings before you have your surgery. Different units may have different advice. A doctor or nurse will check your general health to make sure there won’t be problems with a general anaesthetic if this is being used.
Read more about types of anaesthetic.
You should have a dental check-up and get any problems dealt with well before your operation because there’s a risk of infection if bacteria from dental problems get into the bloodstream.
Recovery
This will vary depending on the type of operation and your general health, so ask your surgeon what to expect. Planning ahead will make things easier when you get home.
Different surgeons have different ideas about the treatment you’ll need after an operation. This is affected by the type of operation and your health. You should discuss with your surgeon what to expect after the operation. Your nurse or physiotherapist will be able to offer support.
After you’ve been discharged from hospital an appointment will be made for you to come in as an outpatient so that your progress can be checked. Sometimes your GP will help with this aftercare. A district nurse may be asked to remove your stitches and change your dressings.
If you stopped taking any of your regular drugs or had to alter the dose before the operation, it’s very important to talk to your rheumatologist for advice on when you should restart your medication.
It’s a good idea to make preparations before the operation. Simple things like choosing clothes that are easy to put on, stocking up your freezer or arranging to have some help at home will all make it easier to manage. It’s a good idea to arrange help with transport because you’ll probably have to attend hospital regularly to see your surgeon, nurse or therapist.
An occupational therapist will be able to advise you before your operation if you have any concerns about coping afterwards. This might be particularly important if your condition affects your upper body and you think you might have difficulty getting around on crutches.
Research and new developments
We're supporting the Outcomes in Ankle Replacement Study (OARS) at the University of East Anglia. The study will provide evidence of how the outcome of total ankle replacement is influenced by:
- the characteristics of the patients undergoing surgery
- the nature of their ankle disease
- the type of implant
- the way in which the patient is managed before and after surgery
This study will also examine the relative costs and benefits of surgery. To collect this information, the researchers will use a newly developed questionnaire called patient-reported outcome measure, or PROM, on 600 people who have undergone ankle replacement surgery. This study will allow a greater understanding of who might benefit most from total ankle replacement for severe ankle disease.