Why do I have pain in my foot or ankle?
Most people experience pain in and around their feet or ankles at some point in their lives.
It’s one of the most complex, hard-working regions of your body. It has 26 bones and 33 small joints, all held together by a network of soft tissue made up of muscles, tendons, ligaments, nerves, and blood vessels.
Most cases of foot or ankle pain are short term and are caused by soft tissue injuries, such as sprains or strains.
These should gradually heal with the help of simple self-care measures. Though some could take a few months to fully recover, you probably won’t need to seek treatment from a healthcare professional.
However, some pain can have no obvious cause or may not improve significantly with self-care.
Pain that seems to be getting worse, does not improve, or lasts longer than a few months could be due to structural changes in the foot or ankle, or an underlying condition.
There can be several explanations for long-term pain in and around the feet or ankles, such as:
- badly fitting footwear
- osteoarthritis
- inflammatory arthritis
- connective tissue diseases
- poor blood circulation
- nerve damage.
How can I treat foot or ankle pain when it starts?
Most foot or ankle pain can be treated without the need to see a healthcare professional.
Soft-tissue injuries should begin to improve over the first few days with the help of some simple self-care tips. You may need to be careful and protect the injured area for several months, until it has fully recovered.
Self-care tips
Paracetamol and pain-relieving gel should help reduce your pain and discomfort.
There are four steps to treating pain, known as RICE therapy, which can help improve healing, particularly in the first 2-3 days, these are:
- Rest – try to avoid putting weight on the injured foot or ankle. Do not exercise, instead try gently moving it from time to time to stop the area getting stiff.
- Ice – put an ice pack or frozen vegetables, covered in a damp cloth, on the painful area for 20 minutes every 2-3 hours.
- Compression – wrap a bandage around the area that’s painful. It should be tight enough to support it, but not so tight that it restricts the blood flow. If you’ve hurt your toe place a small piece of cotton wool between it and the next toe, then tape them together.
- Elevate your foot to reduce swelling.
By gently massaging the painful area from time to time you can help reduce swelling and increase blood flow.
It is best to avoid hot baths, heat packs, ibuprofen, and alcohol in the first few days, as they can affect healing.
Exercise
Exercise can help reduce pain and stiffness in the feet and ankles. You can find examples of exercises that could help you on our exercises for the toes, feet and ankles page.
If your feet or ankles are stiff in the morning you may find it easier to exercise once they have had time to loosen up. A warm bath or shower can help ease stiffness.
Start gently and slowly build up the amount you are doing once each exercise becomes easier or more comfortable.
It’s normal to feel some slight aches as you move your foot or ankle. However, if movement makes it feel worse or is causing bursts of more intense pain, stop and consult a healthcare professional.
Related information
-
Let's Move with Leon
Sign up to Let’s Move with Leon our weekly email programme of 30-minute movement sessions, presented by fitness expert Leon Wormley.
-
Let's Move
Sign up to Let’s Move to receive a wide range of content about moving with arthritis – from exercise videos to stories and interviews with experts – straight to your email inbox.
When should I see a healthcare professional about foot or ankle pain?
Some foot pain can become more than a short-term problem. If you cannot treat the pain yourself or you have a condition that could affect the joints or soft tissue, it may need further investigation.
You should speak to your doctor or a footcare specialist if:
- your pain does not improve in the first few days
- your pain is getting worse
- it is still causing problems after two weeks of self-care
- you have sores that are not healing
- your skin has changed colour – especially if it’s turned dark blue or black
- your foot has changed shape or is really swollen
- you have a high temperature or feel hot and shivery
- it is red, warm, or swollen – as you may have an infection
- the problem keeps coming back or lasts longer than three months
- you have an inflammatory condition, such as rheumatoid arthritis or scleroderma
- you have diabetes
- you are taking steroids, biologics or other drugs that affect your immune system.
Your doctor may want to refer you to a specialist in foot care, such as a podiatrist, physiotherapist, or an orthotist, for a diagnosis and treatment.
Who can help my foot or ankle pain?
There are trained healthcare professionals who specialise in diagnosing and treating problems affecting the foot and lower leg.
A podiatrist
Podiatrists are trained foot specialists, they used to be called chiropodists. They can offer you:
- advice on padding, dressings, specialist insoles, splints and supports
- advice about footwear and exercise
- small non-surgical procedures
- advice on medication
Different areas have different rules for who can be referred to an NHS podiatrist. Some only refer people if they have rheumatoid arthritis, diabetes, or peripheral arterial disease. Other authorities may have broader terms.
If you visit a podiatrist privately you will need to pay for your appointments and any treatment. However, they can refer you for some services, such as scans or x-rays, on the NHS.
You can find a private podiatrist by visiting:
- the Institute of Chiropodists and Podiatrists or calling 01704 546141
- the College of Podiatry
A physiotherapist
Physiotherapists are trained to use movement, exercise, manual therapy, and advice to help get your foot and ankle moving again. They will show you exercises to practice at home to support your recovery.
In some areas you can self-refer to an NHS physiotherapist. Otherwise, your doctor will request an appointment for you.
You can see a physiotherapist privately, though you would have to pay for your treatment. To find a registered private physiotherapist visit the Chartered Society of Physiotherapy.
An orthotist
Orthotists are trained to assess and treat problems in the foot and ankle by using specially made braces, splints, callipers, insoles, and footwear. Usually you need to be referred to an orthotist.
All orthotists, physiotherapists, and podiatrists must be registered with the Health and Care Professions Council (HCPC). You should visit this website to check a practitioner’s credentials.
How are foot or ankle problems diagnosed?
A healthcare professional will usually make their diagnosis after examining your feet. They will look for signs of swelling and any structural changes that could be causing the pain. You may also be asked to walk about, to see whether the problem affects your movement and posture.
Most of the time they can make a diagnosis without scans, x-rays or blood tests, unless they think your pain is being caused by a condition, such as arthritis.
Common causes of foot or ankle pain
Beyond obvious injury, there are several common causes of foot pain. Many of these problems can be diagnosed by the specific areas in the foot or ankle they affect.
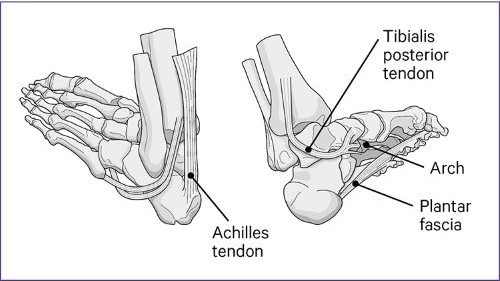
Below shows the main structures affected by foot pain.
Achilles tendinopathy
Achilles tendinopathy is caused by damage or inflammation in the tendon that runs from the calf to the heel bone.
Tendons are strong cords that connect muscles to bones, and support the structure and movement of your feet and ankles.
The main symptoms are:
- pain in the Achilles tendon which worsens after activity
- difficulty moving the foot up and down
- a grating sensation
- swelling, redness or heat around the tendon
- a lump on the tendon.
It commonly affects people who:
- do sports involving a lot of running or jumping
- have some types of inflammatory arthritis
- have high or low arches.
Achilles tendinopathy can take anywhere from a few weeks to several months to fully recover. However, the self-care tips outlined above should help relieve your symptoms.
Tibialis posterior dysfunction
Tibialis posterior dysfunction causes pain, redness, warmth and swelling in the tendon that connects the inside of the calf to the arch of the foot. Your ankle or heel may feel weak and it can cause the arch of your foot to drop.
It can make walking, standing for long periods of time, or rising to your tip toes difficult. It can feel worse when you are active, particularly if you are running or jumping.
It is caused by inflammation, damage or a weakness which over-stretches the tendon. If left untreated, it can eventually make the arch of the foot collapse.
The self-care tips listed above should help with your recovery. However, if the pain is severe or has not improved after two weeks speak to a healthcare professional.
Plantar fasciitis
Plantar fasciitis commonly causes pain in the centre and inner side of the heel.
It's caused by damage to the strong band of tissue, called the plantar fascia, which runs from the heel to the base of the toes.
The plantar fascia should support the arch and help to spread your weight evenly through your foot, so you can walk, run, or stand without difficulty.
However, plantar fasciitis can make it difficult and painful to use your foot properly, particularly just after rest or following activity.
It can increase the risk of lumps of calcium growing on the heel bone, called bone spurs, which could cause more pain when you move the joint.
The self-care tips should help your plantar fascia heal, though it could take up to 18 months to fully recover. Speak to a healthcare professional if you feel no improvement after two weeks.
Bursitis in the foot or ankle
Bursitis causes pain and inflammation, commonly around hard-working joints such as in the big toe, ball of the foot, heel, or ankle. It can also affect any part of the body.
It is caused by swelling in a small pocket of fluid, known as a bursa, or bursae if more than one is affected. Normally these small pouches cushion and protect your bones, joints, and tendons from impact, rubbing or pressure.
However, repeated rubbing, friction, excessive pressure, or injury can cause the fluid inside to increase making the affected bursa inflamed and tender.
For example, you can get bursitis between your ankle and heel if you keep wearing shoes that rub, pinch, or press down on the area. Shoes that are too tight and high heels regularly cause bursitis.
It often appears as a red, painful, swollen lump. However, it can also cause general swelling that you only notice because of the pain, for instance on the bottom of your heel.
People with bunions or irritated joints can be prone to bursitis. Rheumatoid arthritis can also cause bursitis, particularly in the ball of the foot.
The self-care tips recommended earlier should help relieve your pain and inflammation. However, instead of bandaging the area, try using adhesive padding on the swelling to protect it from further friction and pressure. Resting it on a cushion can also help.
If you find self-care treatments are not helping speak to a healthcare professional.
Changes in the shape of your arch
The arch is the inside mid-section of your foot. It determines how your bodyweight is spread and carried by the bones and joints of your feet.
For your foot to function at its best the arch should form a smooth arc from the ball of the foot to the heel.
The height of your arch may never cause you any kind of problems. Some people are born with arches that are higher or lower than average and their bodies adapt to them.
Other people may find their arch shape alters because of complications such as arthritis, weight, pregnancy, or injury. These changes can make you more likely to develop further problems in other parts of your foot, ankle, knee, hip and back.
If you are in pain and think your arch shape has changed speak to a healthcare professional about treatments. Insoles or supports made specially for your foot shape by an orthotist could improve pain caused by high or low arches.
Low arches
A low arch can affect how your foot and ankle works and bears weight. For example, it can make you lean in on your ankle and force your heel to spread outwards.
It can put more strain on your feet, ankles, knees, hips and back. People who naturally have flat feet are less likely to experience problems in these areas because their bodies adapt to their natural arch shape.
However, arches that fall or drop from their normal shape can make you more likely to get overuse injuries. Your body posture or balance may also change, which can increase the strain on your legs, knees, hips and back.
The condition valgus heel, where the ankle leans inwards at an angle causing the heel to drift outward, is often linked to low arches. People with rheumatoid arthritis often develop it because of changes in their joints.
High arches
People with high arches are more likely to walk on the outer edge of their feet because their arches push their feet and ankles outwards. It can put excessive strain on the ankle, heel, and ball of the foot, increasing the risk of problems such as plantar fasciitis.
Problems linked to low and high arches
Arches that are higher or lower than average can increase your risk of developing other problems, such as:
- valgus heel
- hammer toes
- retracted toes
- clawed toes
- mallet toes
- bunions
- corns and calluses.
The self-care tips can help ease pain in your arches.
Changing your footwear to a well-made running trainer that you feel supports the shape of your arch may prevent further painful changes to the structure of your arches.
Insoles and arch supports can help but it’s best to visit a foot specialist, such as a podiatrist, to get ones designed specifically for your foot shape.
If you’re buying new footwear it’s best to take any adaptations, such as insoles, padding, or arch supports with you, as you may need a larger shoe size to fit them in comfortably.
Losing weight, if you need to, can reduce the strain on your arches and may prevent further long-term changes.
You may find it difficult to do exercises that put a lot of pressure through your feet. Swimming is a good way to improve and maintain your fitness because the water supports your body weight.
Other causes of foot pain
Pain in the foot can be a consequence of damage, pressure or rubbing over a long period of time.
Wearing badly fitting shoes, pregnancy, injury, or putting too much strain through specific parts of your foot can all cause changes in the shape of your feet. Often, these changes are painful and can affect your ability to do things.
Sometimes, it’s our choice of shoes that has the biggest impact on the structure of our feet and the problems we develop, such as:
Calluses
Calluses are patches of rough, hard, slightly raised skin that build up on your feet, particularly on points that take the most pressure or rubbing. These patches can be more sensitive and ache more than other parts of your foot. They can be controlled by gently filing the area each week with a pumice or special foot file. If they are left, they can turn into corns.
Corns
Corns are raised areas of hard, knobbly skin which develop where calluses have been left untreated. They often cause a burning sensation. A corn is a permanent change to your foot which will need care and management to stop it becoming too painful. You can manage corns by gently filing or pumicing them each week. You should never cut the skin with a blade.
Corns and calluses will usually grow back within four to six weeks unless you reduce the pressure on the area. Wearing softer, roomier footwear and placing a cushioned pad over the corn or callus can help.
Neuroma
A neuroma causes sudden shooting, stabbing, or burning pain. Most commonly it affects the third and fourth toes and the ball of your foot. It can feel like there is a small stone under your foot and your toes may become numb or tingly. It is caused by a damaged or irritated nerve and often becomes more painful over time. It is also known as Morton’s neuroma and can be made worse by:
- tight, pointy, or high-heeled shoes
- shoes or trainers that put excessive pressure on the ball of your foot and toes.
Athletes and people with low or high arches, bunions or hammer toes commonly get neuromas.
You can ease the pressure on the neuroma by placing a cushioned pad on it. Using soft insoles and wearing wide, comfortable shoes with a low heel and a soft sole can also help. If it continues to cause problems your doctor or a podiatrist can recommend further treatments.
Bunions
A bunion is a bony lump that develops on the side of the joint at the bottom of the big toe. It can change the shape of the joint making it bigger, so it sticks out more. This is called hallux valgus. In extremes it can alter the angle of your big toe, making it bend towards your other toes. You may find your big toe loses flexibility and becomes stiff, which is known as hallux rigidus.
Soft, wide-fitting shoes reduce the pressure on the joint. Bunion pads and insoles can also help relieve pain around the joint, ask a pharmacist for advice. Speak to your doctor if it continues to cause problems.
Clawed, mallet, retracted and hammer toes
Clawed, mallet, retracted or hammer toes are conditions that cause the toes to curl or lift out of line. The main difference between each condition is the joints that are affected in the toe. However, they tend to be treated the same way. These conditions are linked to several other foot problems, including bunions, flat feet, high arches, tendon problems and badly fitting shoes that squash your feet. Arthritis and problems with the nerves in the foot can also cause them.
Hard skin can build-up over the raised toe joints making them uncomfortable and more prone to sores, calluses, and corns.
You can manage these problems by wearing soft, cushioned, wide-fitting shoes, using insoles and applying padding to the painful area. Paracetamol, ibuprofen and pain-relief gels or creams can also help.
Your doctor or a podiatrist may recommend using rubber, leather or silicone splints to relieve your discomfort. However, these changes in the toes can only be permanently corrected with surgery.
Sores
Changes in the structure of the foot can make you more likely to get blisters or open sores. It is important to keep wounds clean and protected with a clean dressing or padding, to stop them getting infected and help them heal.
Also known as ulcers, these wounds can be particularly problematic for people with conditions such as:
Some sores may not heal without specialist treatment and in extreme cases they could cause an infection in the bone, called osteomyelitis. It’s important to tell your rheumatology team about any wounds.
How can arthritis affect your feet?
Several types of arthritis can affect your feet and ankles. Some, such as osteoarthritis, can be managed with painkillers, non-steroidal anti-inflammatory drugs (NSAIDs) and exercises that strengthen and stretch the soft tissue around the affected joint.
If your pain doesn't improve, your doctor may recommend a steroid injection into the joint to reduce the swelling and pain and get your foot and ankle moving more.
However, inflammatory conditions such as rheumatoid arthritis are likely to need disease-modifying anti-rheumatic drugs (DMARDs) or biologics. These long-term treatments should address the inflammation causing your pain.
Osteoarthritis
Osteoarthritis can affect any joint in your foot or ankle, making it painful and swollen at times. It can cause new bone to grow in and around the joint, which changes the shape of your foot, often making the joint look larger and more knobbly.
When it affects the joint at the base of the big toe you may develop a bunion. If it affects your little toe it can cause a small lump, called a bunionette, to appear on the joint at the base of the toe.
Inflammatory conditions
Inflammatory arthritis causes swelling, pain, heat, and redness around the joints, which can affect your whole foot.
There are several types of arthritis that are described as inflammatory conditions.
These conditions can cause sores to appear on your feet which may take a long time to heal or may keep getting worse. If you do get sores speak to your doctor as soon as possible as they could become infected.
Inflammatory arthritis can usually be diagnosed by a physical examination of your joints, blood tests or scans. There are several types that commonly affect different parts of your feet, including:
Rheumatoid arthritis
Rheumatoid arthritis is an autoimmune condition that can affect any joint in the feet, and occasionally, the ankles. It is caused by a fault in the immune system, which makes it attack healthy cells in your body, as if they were germs or viruses. When this happens in and around a joint it can make it swollen, stiff, hot, and painful. It can cause long-term damage to the affected joints in your feet or ankles.
It’s not uncommon for people with rheumatoid arthritis to get painful pea-sized lumps, called nodules, in their heels, toes and soles of their feet.
Psoriatic arthritis and reactive arthritis
Psoriatic arthritis and reactive arthritis are both triggered by an over-reaction in the immune system. They are often linked to plantar fasciitis and Achilles tendinopathy, which cause pain along the back and underside of the heel. They can also cause a condition known as dactylitis, or sausage toe. This makes the entire length of one or two of your toes swollen, painful and difficult to move.
Reactive arthritis usually lasts a relatively short amount of time, often between six to twelve months at most. Whereas psoriatic arthritis tends to need long-term management.
Ankylosing spondylitis
Ankylosing spondylitis commonly affects the lower back but can also cause pain in the heels increasing your risk of developing conditions such as plantar fasciitis and Achilles tendinopathy.
Gout
Gout is a very painful type of arthritis. It is caused by crystals collecting inside a joint and commonly affects the foot, particularly the big toe.
During a gout attack the joint can be inflamed for up to two weeks. Without medication, further attacks can cause permanent damage to the joint, which could then lead to osteoarthritis.
Other arthritis-related conditions that can affect feet
Lupus sometimes affects your joints and tendons making the toes drift outwards and the arches flatten. This can be painful and may make your feet feel stiff after periods of rest.
Raynaud’s phenomenon can occur on its own or with rheumatoid arthritis, scleroderma, or lupus. It makes your toes feel cold, numb, and painful. They may change colour from white, to blue, then red.
These sensations usually stop when your feet warm up. However, going from cold to hot too quickly can make your pain worse. Wearing warm socks or silver lined socks may help prevent these painful attacks.
Raynaud’s can also cause painful sores, known as chilblains, on your toes.
Surgery
Surgery is usually a last option if self-care, exercise, and specialist treatment do not help.
Most foot or ankle surgery aims to correct the position of the joints by resetting the bones or fusing a joint in the corrected position.
An operation may be recommended to:
- correct valgus heel or hammer toes
- remove a neuroma or rheumatoid nodules
- remove part of the bone from a bunion and reshape the toes
- relieve pain.
Joint replacements for the ankle and foot are not yet as successful as knee or hip replacements.
Your doctor will tell you if surgery could help.
Complementary treatments
As long as you don’t have any open wounds, sores or new inflammation in your feet a therapeutic massage and a warm-water footbath can help reduce pain or tiredness in your feet.
There is no current evidence that complementary adaptations, such as magnetic insoles, are better than using standard, cushioned insoles or well-fitted footwear that properly support and protect your feet.
You should talk to your doctor before starting any new complementary treatments in case they conflict with medication you are already taking. If you do use alternative treatments make sure the practitioner is registered, has an ethical code, and is fully insured.
Be critical of what the treatment is doing for you and base your decision to continue upon whether you notice any improvement.