What is ankylosing spondylitis?
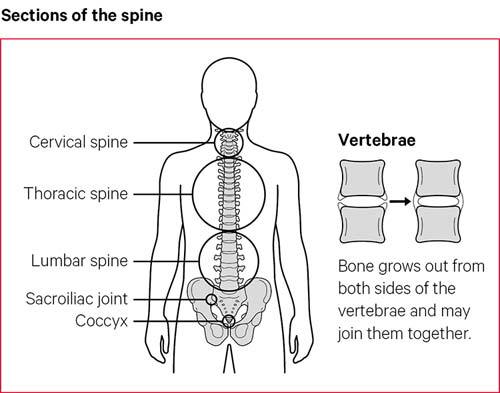
Ankylosing spondylitis (AS) (ank-ee-lo-zing spon-dee-li-tus) is a type of arthritis that mainly affects the back, by causing inflammation in the spine. This can make your back, rib cage and neck stiff and painful.
It often starts in people who are in their late teens or 20s.
In response to the inflammation, the body produces extra calcium around the bones of the spine. This can make extra bits of bone grow and cause your back and neck to be more stiff.
In rare cases some of the bones of the spine may link up, or fuse together because of the extra calcium. In serious cases this can make the spine curve forward more. You can reduce the risk of this happening, if you:
- keep active
- have effective medical treatment
- try to maintain a good posture.
While it mainly affects the neck and back, it can also cause pain and stiffness elsewhere in the body, including in the hips, shoulders and feet.
We don’t yet know what causes ankylosing spondylitis. To some extent it’s related to your genes, but the condition isn’t passed directly from a parent to their children. You can’t catch it from anyone else.
Conditions related to ankylosing spondylitis
Ankylosing spondylitis is a type of spondyloarthritis (spon-dee-lo-arth-rye-tus). This is the name for a group of conditions with similar symptoms – mainly pain and stiffness around the spine.
Here are some other types of spondyloarthritis:
- Non-radiographic (non-radio-graff-ick) axial spondyloarthritis – the main symptoms are similar to ankylosing spondylitis – pain and stiffness around the spine. But there won’t be physical changes to the back that can be seen on an x-ray. Some people with this condition are later diagnosed with ankylosing spondylitis.
- Psoriatic (sorry-at-ick) spondyloarthritis is a form of psoriatic arthritis that can occur alongside the skin condition psoriasis. People with psoriasis can get red, scaly patches of skin.
- Spondyloarthritis associated with inflammatory bowel disease, which is also called enteropathic (en-tur-o-path-ick) arthritis. This is related to bowel conditions such as Crohn’s disease or ulcerative colitis. The bowel is part of the digestive system that helps to break down the food we eat.
- Reactive arthritis is diagnosed when your arthritis is a reaction to an infection.
- Enthesitis (en-thur-si-tus)-related juvenile idiopathic arthritis is the name used when children and teenagers develop inflammation in entheses, the sites where tendons and ligaments attach to bones.
The rest of this content refers to ankylosing spondylitis. However, the treatment and self-management advice is very similar for people with other types of spondyloarthritis.
Symptoms
In the early stages, ankylosing spondylitis is likely to cause::
- stiffness and pain in your lower back in the early morning that lasts at least 30 minutes and then eases through the day or with activity
- pain that wakes you in the night
- pain in one or both buttocks and sometimes the backs of the thighs.
The condition can sometimes be mistaken for common backache.
Common backache often comes in short and painful spells. But the pain from ankylosing spondylitis is likely to be long lasting.
You may also have neck, shoulder, hip or thigh pain, which is worse when you’ve not been active for a time, for example if you sit for long periods working at a desk. Some people have pain, stiffness and swelling in their knees or ankles.
The pain and stiffness can vary over time. If most of the spine is affected, it can cause difficulty with activities that involve bending, twisting or turning.
Other possible symptoms include:
- soreness at the heel or in the arch of your foot
- pain and swelling in a finger or toe
- tenderness at the base of your pelvis, which can make sitting on a hard chair uncomfortable
- chest pain or a tightness around the chest that comes on gradually. This can make it difficult to take deep breaths. Your ribs may feel very tender, and you may find that you’re short of breath after even gentle activity. Coughing or sneezing may cause discomfort or pain.
- inflammation of the bowel. People with ankylosing spondylitis can develop bowel problems known as inflammatory bowel disease (IBD) or colitis. It’s a good idea to see your doctor if you have diarrhoea for more than two weeks or have bloody or slimy poos.
- fatigue, which is severe tiredness that doesn’t improve with sleep or rest. This can be caused by the condition itself, as well as by anaemia. This is when people have a lack of red blood cells, which carry oxygen around the body.
- depression and anxiety.
- inflammation of the eye, called either uveitis or iritis. The first signs are usually a painful and sometimes red eye. It may become uncomfortable to look at bright lights.
If one or both of your eyes are painful or red, or if you have changes to your vision such as partial loss of sight, blurred vision, floaters or sensitivity to light, it’s very important to get medical help as soon as possible. The best place to go is an eye casualty department. Your optician will be able to tell you where the nearest one is. You could also go to a GP surgery or an accident and emergency department. Treatment is usually with steroid eye drops, which are generally very effective.
Complications
If you’ve had ankylosing spondylitis for a long time or if the bones in your back have fused together, you may be at risk of bones in your back fracturing. A fractured bone in your spine can cause nerve damage.
It’s very important that a doctor treating you following a fall or an accident knows that you have ankylosing spondylitis.
If you have new unexplained pain in your spine or new weakness, numbness or tingling in your arms or legs, it’s very important to tell a doctor.
Some people with ankylosing spondylitis develop osteoporosis, a condition that causes bones to thin and be more likely to fracture.
If you have ankylosing spondylitis, or any kind of spondyloarthritis, it can make you slightly more at risk of problems such as a heart attack or a stroke. Taking drugs to reduce inflammation, as well as eating a healthy diet, not smoking and exercising regularly will reduce this risk.
Rarely, the top of your lungs may become scarred if your chest is affected by ankylosing spondylitis.
Although these problems can happen in people with ankylosing spondylitis, they are rare.
Diagnosis
Symptoms of ankylosing spondylitis can be similar to more common back problems, especially in the early stages.
Because of this, many people put up with the pain for some time before seeking help. It’s important to see a doctor as soon as possible if you suspect you have ankylosing spondylitis.
It’s usually diagnosed by a rheumatologist, these are doctors who specialise in conditions affecting the joints, bones and muscles.
There is no one test that can show for certain that you have ankylosing spondylitis. A diagnosis will be made based on several things, including:
- the history of your condition and the symptoms you’ve experienced, including whether pain and discomfort is waking you up during the second half of the night
- a physical examination
- blood tests, which may show inflammation
- x-rays or a magnetic resonance imaging (MRI) scan
- your age. It can be diagnosed at any age, but most often begins before the age of 40, and often much younger.
There are disease activity and pain scores that can help doctors diagnose ankylosing spondylitis. Your doctor will ask if you have key symptoms, such as swollen and painful joints, especially around the spine, and fatigue. You’ll be asked if you have pain in the mornings and how long for. Your answer to these questions could help lead to a diagnosis.
Blood tests can confirm whether you have the HLA-B27 gene. Most people with ankylosing spondylitis test positive for HLA-B27, but so do many people who don’t have the condition. A positive test may point to someone having ankylosing spondylitis, but it won’t confirm the diagnosis.
Treatment
A number of treatments can slow it down and treat pain and stiffness. Exercise and close attention to your posture are just as important to keep your spine mobile and help you to live a normal life.
Some of the drugs below can only be prescribed by a rheumatology consultant.
Drug treatments
Painkillers and non-steroidal anti-inflammatory drugs (NSAIDs)
Painkillers, such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are usually the first choice of treatment for ankylosing spondylitis.
For people who have symptoms that can’t be controlled by anti-inflammatories, other drugs are available to help reduce pain or limit the effects of the condition.
Disease-modifying anti-rheumatic drugs (DMARDs)
Drugs such as sulfasalazine and methotrexate, can treat arthritis in your arms and legs, although they’re not usually effective for spinal symptoms.
These drugs, called disease-modifying anti-rheumatic drugs (DMARDs), can reduce the amount of inflammation that happens in your body. This means that as well as treating symptoms, they can help prevent joint damage.
These drugs can sometimes take several weeks or months to take effect. When they do take effect, they can make a big difference to your pain and stiffness. They’re often long-term treatments.
When taking DMARDs, you’ll need regular check-ups and blood tests to monitor their effect.
Biological therapies
Biological therapies are newer treatments that can be very effective for some people with ankylosing spondylitis and related conditions.
These drugs have a more targeted approach to stop inflammation than the older DMARDs.
They aren’t suitable for everyone and can only be prescribed if your condition can’t be controlled with anti-inflammatory drugs and physiotherapy.
There are a group of biological therapies called anti-TNF drugs. The following can treat ankylosing spondylitis:
Secukinumab is a different type of biological therapy that can also treat ankylosing spondylitis. It’s one of a new family of biological therapies called interleukin, or IL-17 inhibitors. This drug also works by reducing or slowing inflammation.
These drugs are given as an injection, which you, or a partner, relative or friend can learn to do.
The effect of biological therapies will be monitored, and you’ll need to complete questionnaires regularly to check how well you’re responding to treatment.
Steroids
Steroids can be used as a short-term treatment for flare-ups. They’re usually given as an injection into a swollen joint or as a slow-release injection into a muscle. They can also treat painful tendons, for example at the heel, although they aren’t repeated too often as they can cause tendon weakness.
Occasionally, you may be given a course of steroid tablets called prednisolone. While these treatments can be very effective at improving pain and stiffness, you may develop side-effects if you use them for long periods.
If you’ve been prescribed steroid tablets, talk to your doctor about the risk of side effects and how you might be able to reduce your chances of getting them. As with any drug, report any side effects to your doctor immediately.
If you develop eye inflammation, it will usually be treated with steroid eye drops. In more severe cases of eye inflammation, steroids may be given as tablets or as an injection into the eye.
Physical therapies
Physiotherapy is a very important part of the treatment for ankylosing spondylitis. A physiotherapist can put together a programme of exercises to improve your muscle strength and help you maintain mobility in your spine and other joints.
It’s especially important to exercise your back and neck to avoid them stiffening into a bent position.
A physiotherapist will advise you on how to maintain good posture and may be able to offer you hydrotherapy, also known as aquatic therapy. This involves specific exercises for the spine, hips and shoulders carried out in a special warm-water pool.
Many people with ankylosing spondylitis find this therapy helpful and continue their programme at their local swimming pool or with their local National Ankylosing Spondylitis Society (NASS) group.
Surgery
Most people with ankylosing spondylitis don’t need surgery, although some people may need a hip or knee replacement if these joints are badly affected. This can get rid of pain and improve mobility.
If you’re concerned about your spine being bent, raise this with your rheumatologist. Any decision about surgery is difficult and should also involve an experienced spinal surgeon. Though it’s very rare for people to need surgery on their back because of ankylosing spondylitis, it can dramatically improve some people’s lives.
Living with ankylosing spondylitis
Medical treatments can help control ankylosing spondylitis. And there are also many things you can do to help improve your symptoms.
Keeping active and paying attention to your posture can greatly help you minimise the long-term effects of this condition.
Keeping active
If you have ankylosing spondylitis, keeping active can really help you manage your condition.
Regular exercise is good for the range of movement of your back and to stop your spine from stiffening. Start slowly and gradually build up the amount of exercise you do.
Too much rest will increase the stiffening in your spine.
If you’re in a lot of pain and finding it difficult to exercise, talk to your doctor or a physiotherapist.
As well as being good for your back, exercise is important for your heart and lungs, and your overall health. It can also lift your mood and boost your confidence.
Specific simple exercises for your back, chest and limbs will help keep them supple. You may find stretching exercises after a hot shower or bath are especially helpful to ease stiffness in the morning.
Try to do at least some exercise each day. Remember you can take painkillers beforehand to help you exercise.
We have examples of exercises to help improve strength and flexibility. Try to do them every day.
Pilates, yoga and t’ai chi may be useful as these can help with posture, strength and flexibility. You can ask your physiotherapist for advice if you have any doubts or questions about a particular activity. If you go to a class, tell the instructor about your condition.
Swimming is one of the best forms of exercise because it uses lots of muscles and joints without jarring them. And the water supports the weight of your body. Swimming provides a great overall workout that improves your strength, stamina and flexibility.
Speak to your physiotherapist or a swimming instructor if you have discomfort when swimming, as a different stroke or slight change to your technique could help.
As an alternative to swimming, your local pool might run aerobic classes in shallow or deep water which you could try.
There are many types of exercise that will help maintain your mobility and improve your overall health. The key is to find something you enjoy as this will help you to keep doing it.
The National Ankylosing Spondylitis Society (NASS) offers regular exercise classes, run by physiotherapists, at various centres around the country. NASS can also provide information about gym-based exercise, an exercise DVD and mobile app.
Work
Most people with ankylosing spondylitis can continue in their jobs. You may need some changes to your working environment or roles you carry out, especially if you have a physically demanding job.
Talking to people at your workplace about your condition is a good idea. This could be your line manager or human resources department. If your organisation has its own occupational health service, or can provide access to one, this could be a very useful avenue for you.
It would be a good idea to ask for a workplace assessment and tell the person carrying it out that you have ankylosing spondylitis.
Because of the Equality Act (2010), by law workplaces have to make sure that a condition such as ankylosing spondylitis doesn’t stop anyone being successful or comfortable at work.
Ankylosing spondylitis isn’t automatically covered under this law but it is if it affects your ability to carry out every-day tasks. This is based on how you would manage if you weren’t taking any medication. A good question to ask yourself therefore would be if you weren’t on any medication would you easily be able to do tasks such as getting dressed on your own?
Your employers may need to make some reasonable adjustments to your working environment to help you carry out your job. However, either you or they can apply to the government for funding for these adjustments under the Access to Work scheme.
Your employer might be able to provide flexible working, such as changing the hours you work or allowing you to work from home for at least some of the week.
It’s important to remember that you have rights and options.
Try to build short spells of exercise into your working day. Walking around and having a stretch at regular intervals will help you. Try not to stay in the same position for too long.
Sex, pregnancy and ankylosing spondylitis
Sex may be painful if you have ankylosing spondylitis. If it is, try taking some painkillers beforehand and experiment with different positions.
Ankylosing spondylitis can make you feel tired, so it’s important your partner understands how your condition affects you. Good communication can help you maintain an active sex life and counselling can sometimes benefit both partners.
It’s fine to use the contraceptive pill if you have ankylosing spondylitis, but you should tell your doctor you’re taking it.
If you’re thinking of starting a family, it’s very important for both men and women with ankylosing spondylitis to discuss medication with a doctor beforehand.
Some drugs such as methotrexate should be stopped several months before a woman tries to get pregnant. Latest research suggests it’s safe for men to take methotrexate when trying for a baby with their partner.
Biological therapies seem to be safe in the earlier stages of pregnancy but are then stopped later in pregnancy.
If you become pregnant while using a conventional DMARD such as methotrexate or a biological therapy, discuss this with your rheumatology team as soon as possible.
Usually, pregnancy doesn’t cause any special problems for the mother or baby, though the symptoms of ankylosing spondylitis may not ease during pregnancy. If your spine is very stiff, it may not be possible to have an epidural during childbirth. This is an injection into the back that stops people feeling pain in part of the body.
If your condition makes it difficult to open your legs, it’s a good idea to think ahead about the delivery and to discuss with the team at your antenatal appointments whether a Caesarean section might be better. This is an operation to deliver a baby through a cut made in a woman’s tummy and womb.
Will my children develop ankylosing spondylitis?
If you have ankylosing spondylitis, there’s a small chance your children will also develop it. The way it runs in families isn’t straightforward, so if you’re thinking of having a baby and are concerned about this, it’s a good idea to talk to your specialist.
Parents with ankylosing spondylitis sometimes ask if their children should have the HLA-B27 test to see whether they might develop the condition in the future. This isn’t recommended because there’s no way of knowing whether a child will develop ankylosing spondylitis even if they do have the gene.
Sleep
Tiredness and night pain can affect people with ankylosing spondylitis. Good quality sleep can help you manage pain better.
There are many positive steps you can take to help you get good sleep. For example:
- having a warm bath before bed
- a hot water bottle or an electric blanket could also be soothing and provide some pain relief
- cutting out food and drinks with caffeine in, such as tea, coffee, cola, energy drinks and chocolate, from midday onwards. Avoid medicine with caffeine during this time too.
- getting into a good routine of going to bed at the same time each evening, and getting up at the same time each morning – even if your sleep was disturbed
- not sleeping during the day, as this can disturb your sleep pattern
- keeping your bedroom clean, tidy and uncluttered, and keeping your bedding clean – as this will help you relax more
- not watching TV, or looking at any type of electrical or computer screen for at least one hour before you go to bed
- not having a big meal in the two hours before you go to bed
- regular exercise, especially exercise that gets you at least a bit out of breath, can help you get good sleep. It’s best not to exercise within two hours of going to bed.
A medium-firm bed will be more comfortable than one that’s too soft, although the mattress should have some give in it so that it moulds to the shape of your spine.
Some people find memory foam mattresses, mattress toppers and pillows helpful to support their body, and in particular the spine.
Your head and neck should stay in line with the rest of your body when you’re in bed. Too many or not enough pillows could strain your neck.
Talk to your doctor if you continue to have problems sleeping.
Feet and footwear
People with ankylosing spondylitis may develop plantar fasciitis, a condition that causes pain in the heel or arch of the foot. If your feet are affected, you may benefit from custom-made insoles inside your shoes. These can also be called orthotics. Such insoles may help keep your lower limbs in the correct position, and relieve pain in your hips, pelvis or lower back.
A podiatrist is a trained foot specialist, who can assess and advise whether you need custom-made insoles. Sorbothane insoles or gel heel cushions can provide padding and may be enough to ease your discomfort. These can be found in your local chemist or sports shop.
Posture
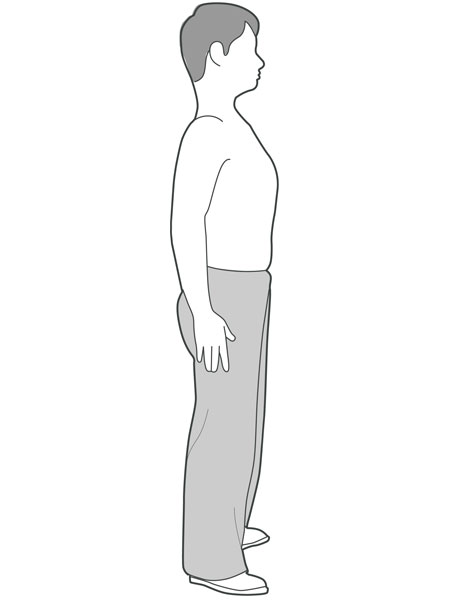
In serious cases ankylosing spondylitis can affect your posture, or the position in which you hold your body. It may cause the spine to bend too much, and this can put extra strain on your spine.
Here are some tips for having a good posture:
- Relax your shoulders and keep them back, rather than hunched forward.
- Keep your chin up.
When sitting down:
- Don’t lean on your elbows.
- Hardback, upright chairs or straight-backed rocking chairs are better for your posture than low, soft, upholstered chairs or sofas.
- When sitting in an office chair, your buttocks should touch the back of your chair.
- Try using a cushion behind your lower back to give extra support or a custom-made lumbar support.
- When working at a computer desk or workstation, don’t stoop or stretch to reach things. Make sure everything you need is within easy reach.
- Make sure your seat is at the correct height.
- Keep your knees at right angles – get a foot rest if you need one.
- Don’t sit in one position for too long without moving your back.
If you can, try to lie on your back on the floor sometime during the day. This will help stretch out the front of your hips and improve your posture. You might like to use pillows to support your head, but try to keep the number of pillows to a minimum. Don’t place a pillow under your knees – stretching your knees out fully helps to maintain flexibility.
A physiotherapist can provide further advice and exercises to help with your posture.
Check your posture
You can check your posture by standing with your back against a flat wall within view of a full-size mirror.
Keep your heels, bottom and shoulders as close as you can to the wall. Hold this position for five seconds and then relax, try to do this three times in a row. Do this regularly, perhaps once a month, and record any differences you notice in the mirror. For example:
- How does your back look?
- Is there change to the natural curve of your spine?
- Can you keep your heels against the wall?
- Note the distance from the back of your head to the wall.
Report any changes you notice to your doctor. If you or someone else can take pictures of you doing this exercise it can help to monitor any change to your posture. Each picture must be taken from exactly the same position and angle every time. If you have difficulties with this exercise, seek advice from your physiotherapist or doctor.
Driving
Driving shouldn’t be a problem if you have ankylosing spondylitis, but there are a few points to bear in mind:
- On a long journey, stop from time to time at a safe place for five minutes and get out of the car for a stretch and quick walk around.
- If your neck or back is very stiff, reversing into parking spaces may be more difficult. Special mirrors and parking sensors can be fitted to help with this. You should inform the Driver & Vehicle Licensing Agency (DVLA) of your condition if you use fitted adaptations.
- If your neck is stiff, it will be more prone to injury. Make sure your headrest is correctly adjusted and that you keep your head back against it.
- If you can’t walk very far, you may be eligible for a Blue Badge, which entitles you to use disabled drivers’ parking spaces.
Your local council can give you information on the Blue Badge parking scheme. The National Ankylosing Spondylitis Society (NASS) can also provide guidance on this and about special mirrors.
Diet and nutrition
No particular foods have been found to make ankylosing spondylitis either better or worse.
However, eating a low-fat, healthy and balanced diet will help you stay a healthy weight for you and is also good for your heart and general health. Being overweight will increase the strain on your back and other joints.
Because ankylosing spondylitis can increase your risk of the condition osteoporosis, which makes bones thinner, it’s important you get enough calcium and vitamin D, to keep your bones healthy.
The best source of vitamin D is from sunshine on the skin. However, because we can’t guarantee sunshine all year round in the UK, it’s recommended we should all take vitamin D supplements daily in the autumn and winter months.
People at risk of not getting enough vitamin D from the sunshine are encouraged to take vitamin D supplements all year round. This includes people who:
- don’t spend much time outdoors
- wear clothes that cover all their skin
- have dark skin, as darker skin is not as good at absorbing vitamin D from sunshine.
Calcium is very important to make strong bones. The best forms of calcium are:
- dairy products such as milk, cheese and yoghurt – low-fat ones are best
- calcium-enriched milks made from soya, rice or oats
- fish that are eaten with the bones, such as tinned sardines.
Many diets have been recommended for people with ankylosing spondylitis, including avoiding certain food types. There’s no convincing evidence that these work, and there’s a chance you could miss out on essential nutrients. If you’re keen to try any of these diets it would be a good idea to discuss it with a dietitian or your doctor first.
Stopping smoking
If you have ankylosing spondylitis and you smoke, stopping smoking would be one of the best things you can do.
Having ankylosing spondylitis, or any kind of spondyloarthritis, can make you more at risk of having a heart attack or stroke. It can also cause problems with the lungs, as it can reduce movement of the joints in the chest.
Smoking is likely to put you more at risk of having a heart or lung problem, and of making them worse. Smoking can make other symptoms of ankylosing spondylitis worse too. There’s also evidence that it can reduce the effectiveness of treatments.
Smoking is more likely to cause the bones in the spine fuse together.
Stopping smoking can be difficult. However, with determination and persistence, you can succeed. Your doctor or rheumatology team will be able to help if you’re struggling to stop smoking. The NHS has information, advice and support online to help.
Complementary medicine
Generally speaking, complementary and alternative treatments are usually safe. However, you should always talk to your doctor before starting treatment, as there are some risks associated with specific therapies. It’s important to go to a legally registered therapist, or one with a set ethical code who is fully insured.
If you decide to try therapies or supplements, you should be critical of what they’re doing for you and base your decision to continue on whether you notice any improvement.
Acupuncture can help relieve pain but won’t have any effect on the way the condition progresses. Very fine needles are inserted at a number of sites around the body but not necessarily at the painful area. Pain relief is obtained by interfering with pain signals to the brain and by causing the release of natural painkillers, called endorphins. To be successful, you might need to have several sessions.
Spinal manipulation is not helpful or safe for people with ankylosing spondylitis as it could result in permanent damage to your spine or spinal cord. Manipulation is a type of manual therapy used to adjust parts of the body, joints and muscles to treat stiffness and deformity. It’s sometimes used in physiotherapy, chiropractic, osteopathy and orthopaedics.
Research and new developments
Previous research has shown that ankylosing spondylitis has a strong genetic component and we’re currently funding several research projects to further understand this. Previously, we part funded research that identified a specific gene, called IL23R, that’s linked to the condition. We’re now funding a follow-on project to investigate how changes in this gene lead to the development of ankylosing spondylitis.
We’re also supporting a study that’s investigating a gene called RUNX3. Researchers are investigating whether this molecule can be targeted with drugs. Results from this research may lead to the development of new and more effective drug treatments.
We’re funding a project investigating the protein HLA-B27. This protein is found in over 90% of people with ankylosing spondylitis. It’s thought that HLA-B27 proteins tend to fold incorrectly inside cells, which may lead to the immune system releasing chemicals that cause inflammation. This research aims to generate HLA-B27 specific treatments that overcome the problems associated with current treatment options.
We’re also supporting research which aims to uncover the link between inflammation of the intestine and ankylosing spondylitis. There’s strong evidence from previous research that the health of the intestine can influence the condition. This research aims to explain how and why this happens, and to identify groups of patients most affected by intestinal inflammation. This could lead to new and improved treatments for this condition.
Exercise
Stand against a wall
Standing with your heels and backside against a wall, push (but don’t tilt) your head back towards the wall. Hold for 5 seconds then relax. Repeat about 10 times if possible.
Waist turn
Stand in an open space with your feet apart. Place your hands on your hips. Turn from the waist to look behind you. Keep your knees and feet facing the front. Hold for 5 seconds. Repeat to the other side, 5 times each side.
Lay down, knees bent, breathe
Lying on your back, knees bent, feet flat on the ground:
(a) Put your hands on your ribs at the sides of your chest. Breathe in deeply through your nose and out through your mouth, pushing your ribs out against your hands as you breathe in. Repeat about 10 times. Remember, it’s as important to breathe out fully as it is to breathe in deeply.
(b) Put your hands on the upper part of the front of your chest. Breathe in deeply through your nose and then breathe out as far as you can through your mouth. Push your ribs up against your hands as you breathe in – again about 10 times. You can do this exercise at any time in a lying or sitting position.

Superman
Lying on your front, looking straight ahead, hands by your sides (if necessary you can put a pillow under your chest to get comfortable).
Raise one leg off the ground keeping your knee straight, about 5 times for each leg. It helps to have the opposite arm stretched out in front of you.
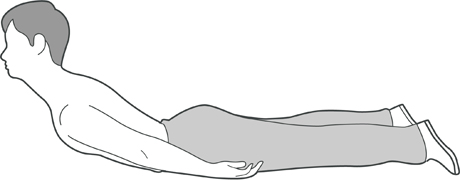
Head and shoulder raise
Lying on your front, looking straight ahead, hands by your sides (if necessary you can put a pillow under your chest to get comfortable):
Raise your head and shoulders off the ground as high as you can – about 10 times.
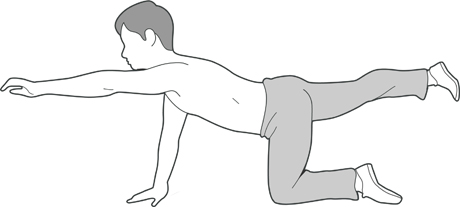
Bird-dog
Kneeling on the floor on all fours, stretch alternate arms and legs out parallel with the floor and hold for 10 seconds. Lower and then repeat with the other arm and leg, 5 times each side.
Ben’s story

I’ve just spent six months living and working in the Amazon rainforest, in the Manu National Park, in Peru.
For the first three months we learned how to recognise different vegetation, animals and reptiles. Then we trained new volunteers.
A big challenge was not having medication out there, the hot and humid climate helped. Hiking in the jungle six days a week was great for my fitness.
I’ve wanted to visit the Amazon for as long as I can remember. It’s one of the most amazing places on the planet, and it lived up to my expectations. But it’s disappearing quickly.
Even though I’m back in the UK, I’m staying off my medication as much as I can. I’m trying to control it through exercise and stretching. I do yoga, which is good for stretching and relaxing. I’ve also started running.
The exercise I did in the jungle was really good. It drove home how important exercise is and no matter how you feel it’s good to do some. In the long run, it will really help.
There were times before I left and when I first started, I considered cancelling the whole thing. Having arthritis and diabetes and going to such a remote place was scary.
I had a lot of self-doubt. Once I’d been out there for a bit, I knew the days that I should say no to doing things, I knew how to manage it.
Life is for living, and you’ve got to make the most of it.
If that means hobbling around a rainforest, a bit of discomfort is worth it for a once-in-a-life time experience.
If you’re young and have a condition like ankylosing spondylitis, you shouldn’t think it’s the end of the world.
The key is to have faith in yourself, that you are strong enough to overcome the obstacles. But also, be realistic and pre-empt what might be difficult and take steps to overcome or avoid potential problems.
It can be difficult, and there will be days when you won’t want to get out of bed, when everything hurts, and it sucks, but you have to break through it.
As soon as you’re up and moving, the adrenalin takes over and it goes to the back of your mind.
I cannot emphasise strongly enough that you should use the people around you for support. It can take a lot of strength to ask for help, but it’s important to.
In Peru I had a lot of support, and I couldn’t have done many things without people’s help. In the jungle my friends carried my bag when we were hiking if my neck or back were hurting.
I made so many friends for life.
For pictures and information of Ben’s travels and work in the Amazon, visit his website.
Related information
Poppy's story

Before I was diagnosed, I felt frustrated. No matter how much I told doctors about the level of pain I was in they kept saying it was growing pains, which I knew it wasn't. I was worried, I had no explanation for why I was feeling this pain and stiffness, or why I was so fatigued.
At its worst, the pain is excruciating. I have been in floods of tears with the pain at two, three, or four in the morning, not knowing what to do. This has a huge psychological effect, it can make me feel like I’m not strong enough to cope and I just wish to be pain free for a day.
But the hardest part is the fatigue. Sometimes it feels as though there are weights attached to my limbs, and it can take every ounce of energy just to walk down the road or to the fridge. You can find yourself being mentally fatigued too, when it feels as though there's a block in your brain, the words want to come out, but they just won't.
Support is so important. My family are amazing. When my injections are due my mum makes sure there's a can of my favourite lemonade in the fridge to help with my nausea. My fiancé Ben is my rock, he sees me when I'm at my worst, when the pain and fatigue are really bad. He has been there from before the diagnosis, and he helped me fight for that diagnosis. I have some amazing friends too who send me lecture notes if I'm not in uni so I don't fall behind.
Despite the AS, I like a sense of normality – of just being a normal 23 year old, as best as I can. I go to uni, I still work, I go to the gym three times a week. Boosting your mental health and keeping positive does help. You also need to listen to your body, you are the only person who knows when you need a rest. Talking to others with AS, people who really understand what you’re going through, that can make a big difference.
A big thing for me was to continue with my third year at university and to graduate. I have had a lot of obstacles this academic year – illness, pain, flares, medication and hospital appointments, but it has all just driven me to carry on and finish.
I have been told to rethink my career choice of teaching as the pressure and workload may have a negative impact on my AS, but these opinions have just made me want to become one more. I know my limits, but I also know that I want to work with children and young people, I always have.
AS won't stand in the way of my aspirations, it just might be that I have to take a different path to get to my end goal, but that's ok.